by Society for Cardiovascular Angiography and Interventions
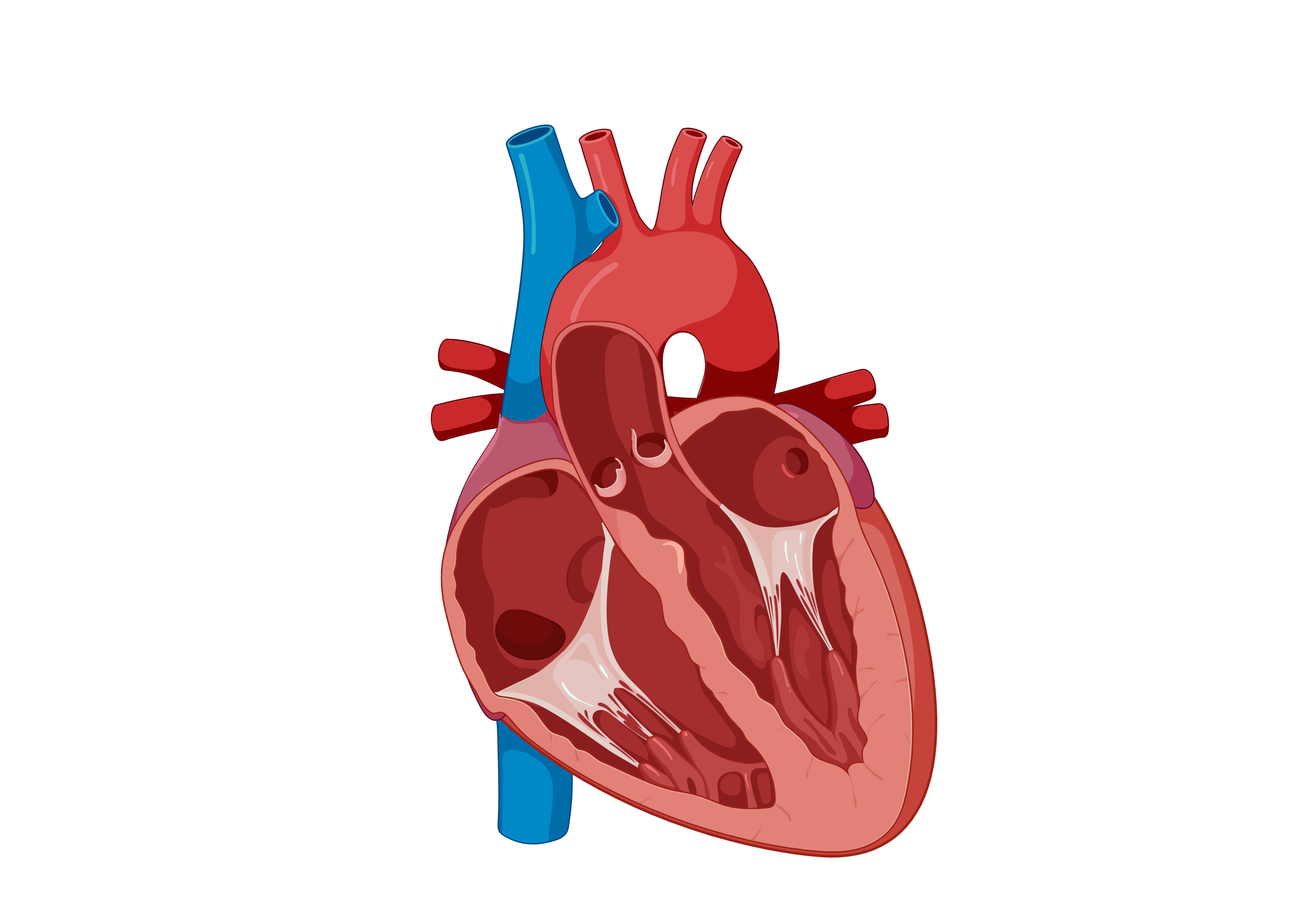
Procedure to access the coronary circulation and blood filled chambers of the heart using a catheter. It is performed for both diagnostic and interventional (treatment) purposes. Credit: Wikimedia Commons, CC BY 3.0 DEED
New data from the CALORI Cardiac Catheterization trial shows significant improvement in patient well-being and satisfaction without compromising safety after implementation of a liberal non-fasting strategy prior to a cardiac catheterization procedures. The late-breaking results were presented today at the Society for Cardiovascular Angiography & Interventions (SCAI) 2024 Scientific Sessions.
More than one million cardiac catheterizations are performed each year in the U.S. to diagnose heart problems. The risk of complications is low, but issues such as bleeding, pain, infections, or blood clots could occur. In addition, routine pre-procedural fasting remains the standard of care, despite a lack of robust evidence to support this practice.
The CALORI Cardiac Catheterization trial focuses on inpatients undergoing elective or urgent cardiac catheterization procedures. This single-center, randomized trial investigated the impact of fasting after midnight versus unrestricted oral intake prior to cardiac catheterization.
The primary endpoint assessed pre-procedural patient satisfaction levels (scaled 0-5, 0 signifying absence of variable and 5 the most extreme form) regarding hunger, fatigue, anxiety, and nausea. Additionally, a composite well-being score, incorporating hunger and fatigue, was utilized. Secondary endpoints encompassed post-procedural satisfaction and the occurrence of peri-procedural adverse events such as emesis, aspiration, or intubation.
Among the 198 patients analyzed (65% male and 42% Black), non-fasting patients showed significantly better composite pre-procedural well-being scores of 2.4 ± 2.4 compared to 6.0 ± 2.5 for those who were withheld from fluids or solids (Nil Per Os, NPO) (p<0.001). Individual scores for hunger (0.9 ± 1.5 vs. 3.7 ± 1.5, p<0.001), fatigue (1.5 ± 1.6 vs. 2.3 ± 1.8, p<0.001), and nausea (0.1 ± 0.5 vs. 0.5 ±1.2, p=0.006) were also significantly better in the non-fasting arm.
Post-procedural satisfaction was significantly higher in the non-fasting group (0.3 ± 0.7 vs. 1.0 ± 1.3, p<0.001). Time from most recent oral intake to procedure start averaged 148 minutes for the non-fasting and 970 minutes for the NPO strategy (p<0.001). Adverse events did not differ between groups.
"Just as our techniques and technology for cardiac catheterization have evolved, so should our approach to pre-procedure management," said Dr. Brian Mitchell, interventional cardiology fellow at Virginia Commonwealth University, and lead author of the study.
"Few studies have prospectively explored this strategy in such a diverse patient population, and with such liberal non-fasting allowances, making it the most comprehensive and generalizable study on this topic to date. Given our findings, we hope that providers will limit pre-procedural fasting to those patients at high risk of aspiration or conversion to general anesthesia."
More information: "Cardiac Catheterization with Liberal Oral Intake: The CALORI trial," Thursday, May 2, 2024; 9:59-10:06 AM PT, scai.org/scai-2024-scientific-sessions
Provided by Society for Cardiovascular Angiography and Interventions




Post comments