
There is a disease that, once contracted, feels as though an uncontrollable "eraser" is inside the brain, slowly wiping away all memories of family, friends, and even oneself—this is Alzheimer's disease.
Patients with Alzheimer's may exhibit abnormal behaviors and emotions: a previously calm and reserved person might start having outbursts, yelling, and even resorting to violence towards those around them. As the disease progresses to its advanced stages, they gradually lose the ability to take care of themselves, slowly regressing to a child-like state.
To this day, Alzheimer's disease remains incurable, and medications can only slow the progression to a certain extent. Therefore, early prevention, detection, and intervention are key.
September 21, 2024, marks the 31st "World Alzheimer's Day." On this occasion, we call on everyone to gain a deeper understanding of the prevention, care, and treatment of this disease, to pay attention to the brain health of ourselves and our families, or to help those around us in need, as we tackle the challenges of prevention, care, and treatment together.
A Quietly Onset and Slowly Worsening Brain Disease
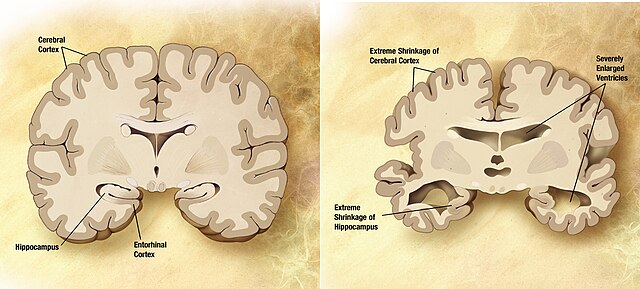
Alzheimer's disease (AD) is a hidden, progressively developing neurodegenerative disorder of the central nervous system, commonly referred to as "senile dementia" because it is the leading cause of dementia in the elderly. It is a brain disease that quietly begins and gradually worsens. By the time symptoms become noticeable, the brain has already undergone irreversible neuronal loss and pathological damage.
Alzheimer's disease is like a "silent farewell" happening inside the brain, gradually and painfully taking away a person's memory, language, thinking, emotions, and ability to move. Medically, it is divided into two stages: pre-dementia and dementia.
Pre-dementia Stage
Also known as mild cognitive impairment (MCI), it is characterized by mild declines in abilities such as learning, attention, executive function, and language. These symptoms may slightly impact daily life, but patients can generally maintain a basic level of independence.
It’s important to intervene early in the disease to potentially pause its progression. If you or a loved one exhibit any of the following 10 signs, don’t ignore them—seek medical attention promptly:
Frequent forgetfulness, particularly a significant decline in remembering recent information, such as forgetting things that were just said, done, or agreed upon.
Inability to complete tasks that were once familiar, such as a driver frequently getting lost or an accountant forgetting how to use familiar accounting software.
Difficulty with language, such as being unable to express thoughts or finding it hard to understand others.
Reduced sense of time and direction, sometimes getting confused about the date or even the time of day, or getting lost in familiar places.
Poor judgment and awareness, making them easy targets for scams, such as lending money to strangers or repeatedly buying unnecessary items.
Misplacing items, like putting fruit in a wardrobe or socks on the dining table, or keeping trash as treasures.
Loss of abstract thinking, such as difficulty organizing tasks or forgetting bank account passwords and amounts.
Unusual emotional or behavioral changes, such as crying or getting angry for no reason, or engaging in out-of-character behaviors like spitting on the ground or taking items from a store without paying.
Personality changes, such as becoming suspicious, fearful, or anxious in a short period.
Loss of interest and reduced ability to act, becoming indifferent or apathetic, losing interest in hobbies, avoiding work or social activities, sitting in front of the TV for hours, or falling into prolonged drowsiness
Dementia Stage
Alzheimer's disease can progress over 10-20 years, during which cognitive decline severely impacts daily life. The dementia stage is divided into three phases based on the severity of cognitive impairment: mild, moderate, and severe.
Mild AD: This stage typically lasts 1-3 years, during which memory loss worsens significantly, and cognitive decline becomes evident in daily activities. Patients may frequently get lost, forget important dates or events, and struggle with managing finances. At this point, timely medication, cognitive training, and family support are crucial in slowing disease progression.
Moderate AD: This stage, lasting 2-10 years, is marked by further cognitive deterioration. Both short- and long-term memory are severely affected, and spatial awareness diminishes. Disorientation regarding time and place worsens. Patients may need assistance with outdoor activities and even personal hygiene, like dressing and bathing. Emotional and personality changes may occur, such as increased suspicion, irritability, or neglect of personal cleanliness. Professional care, psychological intervention, and the patience and understanding of family members become essential at this stage.
Severe AD: As the disease severely damages the central nervous system, patients enter a state of total cognitive decline, losing nearly all memory and cognitive functions. They can no longer perform daily tasks independently and may experience incontinence, muteness, and limb rigidity. Worse, long-term bedridden patients are prone to complications like lung infections, urinary tract infections, and pressure sores, which often lead to death in Alzheimer's patients.
How to Effectively Prevent Alzheimer's in Daily Life?
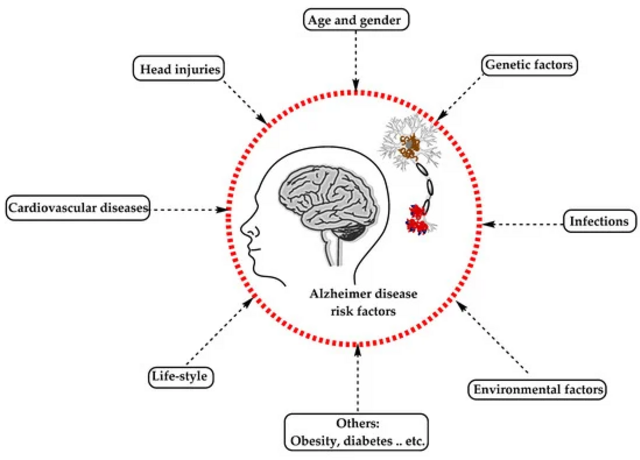
Alzheimer's disease is a complex condition caused by a combination of genetic, lifestyle, and environmental factors. Part of it is triggered by specific genetic changes, though the exact mechanisms of the disease are still not fully understood.
Aging is widely recognized as a significant risk factor for Alzheimer's, with older individuals being more susceptible to the disease. The World Health Organization (WHO) estimates that the prevalence of Alzheimer's disease among people over 65 years old globally is between 4% and 7%. The risk of developing Alzheimer's doubles with every 6.1-year increase in age, and for those over 85, the prevalence can reach as high as 20% to 30%.
Upon reading this, people often develop two common misconceptions about Alzheimer's disease:
Misconception 1: Memory decline in the elderly is normal aging?
Normal aging may cause occasional forgetfulness, such as forgetting familiar people or planned events, but this type of memory loss is usually temporary, and the person can recall the information naturally without any lasting impact on cognitive function or daily life. In contrast, Alzheimer's disease not only leads to memory deterioration and slower reactions but, if left untreated, can progressively cause a loss of cognitive abilities and self-care skills. Ultimately, this can not only affect the patient’s quality of life but may also shorten their natural lifespan. Therefore, Alzheimer's disease is not a normal part of aging—it's a real illness of the brain.
Misconception 2: Should Alzheimer's disease prevention only begin in old age?
Scientific research indicates that the pathological changes of Alzheimer's disease begin 10 to 20 years before any noticeable cognitive decline. This means that during a person’s thirties or forties, the disease may already be developing in the brain, even though no symptoms are present at this stage, making it difficult to detect. Therefore, starting in your twenties, it’s important to consciously begin taking steps to prevent Alzheimer's by reducing exposure to causes and risk factors and strengthening individual resistance, which can effectively prevent or delay the onset of the disease.
The internationally renowned medical journal The Lancet lists 14 preventable and controllable risk factors, including lack of physical activity, smoking, excessive alcohol consumption, air pollution, lack of social interaction, obesity, hearing loss, depression, diabetes, high blood pressure, low educational attainment, brain injury, impaired vision, and abnormal levels of HDL/LDL cholesterol.
Accordingly, early prevention can start from the following aspects:
1. Adjusting Lifestyle Habits
Regular Exercise: Consistent and moderate-to-high intensity exercise can reduce the risk of cognitive decline. It is recommended to engage in at least 150 minutes of aerobic exercise per week. Elderly individuals can choose suitable activities based on their health, such as walking, Tai Chi, or Baduanjin.
Adequate Sleep: Insomnia is a risk factor for cognitive impairment. To prevent cognitive decline, it is recommended to maintain 6-8 hours of quality sleep daily.
Healthy Diet: A balanced intake of nutrients is essential. Health-conscious diets such as the Mediterranean, DASH, and MIND diets have been shown to slow cognitive decline in older adults.
Weight Management: Maintaining a healthy weight is crucial to avoiding both overweight and underweight conditions, as well as malnutrition. It is also important to actively prevent and treat chronic diseases such as hyperlipidemia and osteoporosis.
Pay Attention to Living Environment: Ensure proper ventilation and live in environments with clean air.
2. Unlocking the Brain’s Potential
Continuous Learning: Regularly engaging with new knowledge can stimulate the brain, helping to delay cognitive decline.
Cognitive Training: Participate in cognitive training that focuses on memory and multiple domains (such as attention, executive function). This can help delay the onset of cognitive impairment.
Mindfulness Meditation: Regular mindfulness meditation can activate the prefrontal cortex, increase gray matter density, and enhance the hippocampus, leading to improvements in attention, memory, learning, and emotional regulation.
3. Health Management and Monitoring
Quit Smoking and Limit Alcohol: Both the 2023 World Alzheimer’s Report published by the International Alzheimer’s Disease Association and the WHO Guidelines for Reducing the Risk of Cognitive Decline and Dementia point out that excessive alcohol consumption and smoking are risk factors for Alzheimer's disease (AD).
Prevent Hypertension and Diabetes: Regularly monitor blood pressure, blood sugar, and cholesterol levels, as these chronic diseases can also negatively affect cognitive function.
Protect the Head: Wear seat belts when driving and helmets when engaging in outdoor activities with a risk of collision to reduce the risk of brain injury.
Pay Attention to Vision and Hearing: Vision and hearing are key senses for perceiving the world. For those experiencing vision or hearing loss, using visual aids, hearing aids, or other supportive devices can help reduce the risk of social isolation.
4. Maintain Mental Health
Stay Socially Active: Studies show that elderly individuals with higher levels of social engagement experience slower cognitive decline. Encourage seniors to actively participate in community activities and volunteer work to avoid social isolation.
Adopt a Positive Attitude: Research has found that repetitive negative thinking is associated with cognitive decline and the accumulation of two harmful proteins linked to AD. Therefore, it’s important to pay close attention to mental health issues such as depression and anxiety, especially elderly depression.




Post comments