Severe joint damage seen with rheumatoid and psoriatic arthritis
By Lana Barhum
Medically reviewed by Marissa Sansone, MD
Fact checked by Sarah Scott
Arthritis mutilans is a severe form of chronic rheumatoid arthritis or psoriatic arthritis and one of the most advanced types of joint disease overall. It is characterized by severe inflammation that damages the joints of the hands and feet, causing deformity and the loss of use. Less commonly, it can affect the spine and lead to changes in posture and mobility. Early and aggressive treatment of arthritis mutilans is important and should start at the time of diagnosis.1
Arthritis mutilans is considered rare, affecting about 4% of people with psoriatic arthritis and around 4.4% of people with rheumatoid arthritis, according to the latest research.23
Causes
Essentially, arthritis mutilans is simply an autoimmune disease turned on high. While all autoimmune diseases are characterized by inflammation, only rheumatoid arthritis and psoriatic arthritis are subject to the extremes seen with arthritis mutilans. Scientists are unsure why this is at this time. Some studies have tried to link it to certain pre-existing conditions such as hypertension but a connection has not been made yet to explain why some people are more susceptible to arthritis mutilans than others.4
Part of the reason may be that rheumatoid arthritis and psoriatic arthritis cause similar types of inflammation. They even need a differential diagnosis to tell one from the other.
Rheumatoid arthritis is defined by an autoimmune assault on the joints, causing pain, swelling, redness, and the gradual restriction of movement.5 It can be diagnosed with blood tests that detect the presence of rheumatoid factor (RF), and anti-cyclic citrullinated peptide (Anti-CCP), autoantibodies found in most people with the disease.
Psoriatic arthritis is an autoimmune disorder integrally linked to psoriasis. Psoriasis specifically targets skin cells, triggering inflammation and the production of dry, scaly lesions.6 Psoriatic arthritis occurs when that inflammation also attacks the joints and surrounding structures.
Psoriasis not only develops differently than rheumatoid arthritis (asymmetrically rather than symmetrically) but also has no blood tests to confirm its presence.
Whatever the underlying cause, rheumatoid arthritis and psoriatic arthritis can both lead to damage and disfigurement in the joints of hands, feet, or spine called arthritis mutilans.7
The inflammation is severe enough to accelerate cartilage and bone mineral loss, leading to a collapse of the joint space. It also causes the buildup of fibrous tissues (known as pannus) around the joint, which is what leads to deformity.8
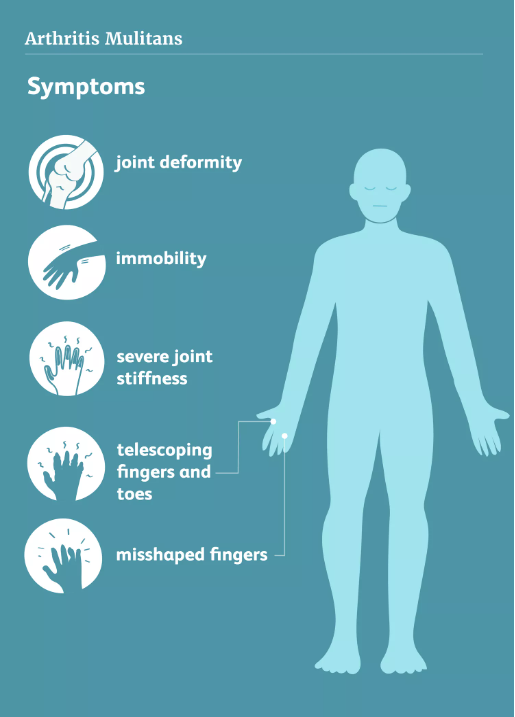
Symptoms
The term mutilans is derived from the Latin for "mutilated" or "maimed." As such, the main symptoms of arthritis mutilans are:9
Joint deformity
Loss in range of motion (ROM)
This can interfere with your ability to perform everyday tasks like fastening buttons and opening jars.
Arthritis mutilans may also lead to "opera-glass hand" in which the connective tissues can no longer support the joints.10 This causes them to retract in a heap-like fashion also known as "telescoping fingers". In some cases, the joints will fuse—a condition referred to as ankylosis—causing immobility and the fixation of the joint.11
Signs of opera-glass hand include:
Fingers that are significantly shortened or stretched
Finger skin that is stretched, wrinkled, and shiny-looking
Others may develop a "pencil-in-cup deformity," so named because on X-ray images the ends of the bones will narrow like the tip of a pencil while the adjoining bone will be worn down into a cup-like shape.12
Diagnosis
Arthritis mutilans is primarily diagnosed with imaging tests such as X-rays and computed tomography (CT). Magnetic resonance imaging (MRI) is far better at imaging soft tissues and is useful in measuring cartilage loss and the formation of pannus.
Blood work can help confirm the underlying cause, measure inflammation, and evaluate disease progression. Results can help direct appropriate medical treatment and monitor your response to it.
Treatment
Early treatment almost always confers to better results, slowing the progression of the disease and maintaining the highest quality of life possible.13
Aggressive physical therapy, especially in the hands, can delay the disease’s progress and halt severe joint damage. Splinting may also help with joint stabilization, but it is typically used for short periods of time to avoid muscle atrophy.
High doses of nonsteroidal anti-inflammatory drugs (NSAIDs) like Advil (ibuprofen) or Celebrex (celecoxib) can help relieve inflammation and pain. Oral and intra-articular injections of corticosteroids can do the same, but are used sparingly to avoid long-term side effects.
Especially severe cases may benefit from tumor necrosis factor (TNF) inhibitor drugs like Humira (adalimumab) and Enbrel (etanercept).14 These biologic drugs help temper the effects of TNF, reducing the overall inflammation that contributes to joint damage.
Surgery may be explored if joint damage interferes with the ability to work or function normally.15 Options include bone grafts to replace lost bone tissue and arthrodesis (joint fusion) to relieve intractable pain.
Coping
Arthritis mutilans can be painful and debilitating, but it doesn't mean you can't take control of your life. A commitment to early and ongoing physical therapy is key. This may include hand therapy, occupational therapy, and even mind-body therapies (like meditation and guided imagery) to reduce stress and your emotional response to pain.16
You should also find support to avoid isolation and depression common in people with arthritis. This may include your medical team, family, friends, or support groups located either online, through community health centers, or via non-profit associations like Creaky Joints.
Good self-care is also important. This includes a healthy diet, routine exercise, and the cessation of smoking. Smoking can interfere with your medications and promote inflammation that accelerates the progression of the disease.
Sources
National Library of Medicine. Psoriatic Arthritis.
Yoshida M, Belt EA, Kaarela K, Kauppi MJ, Shimamura T. Prevalence of mutilans-like hand deformities in patients with seropositive rheumatoid arthritis. A prospective 20-year study. Scand J Rheumatol. 1999;28(1):38-40. doi:10.1080/03009749950155760
Rech J, Sticherling M, Stoessel D, Biermann MHC, Häberle BM, Reinhardt M. Psoriatic arthritis epidemiology, comorbid disease profiles and risk factors: results from a claims database analysis. Rheumatol Adv Pract. 2020;4(2):rkaa033. doi:10.1093/rap/rkaa033
Mistegård J, Gudbjornsson B, Lindqvist U, et al. Comorbidities in a Cohort of 66 Patients With Psoriatic Arthritis Mutilans-Results From the Nordic PAM Study. Front Med (Lausanne). 2021;8:629741. doi:10.3389/fmed.2021.629741
Johns Hopkins University Arthritis Center. Rheumatoid Arthritis Signs and Symptoms.
Sakkas LI, Bogdanos DP. Are psoriasis and psoriatic arthritis the same disease? The IL-23/IL-17 axis data. Autoimmun Rev. 2017;16(1):10-15. doi:10.1016/j.autrev.2016.09.015
Mochizuki T, Ikari K, Okazaki K. Delayed Diagnosis of Psoriatic Arthritis Mutilans due to Arthritis Prior to Skin Lesion. Case Rep Rheumatol. 2018;2018:4216938. doi:10.1155/2018/4216938
Shiraishi M, Fukuda T, Igarashi T, Tokashiki T, Kayama R, Ojiri H. Differentiating rheumatoid and psoriatic arthritis of the hand: multimodality imaging characteristics. RadioGraphics. 2020;40(5):1339-1354. doi:10.1148/rg.2020200029
National Library of Medicine. Arthritis.
The American College of Foot and Orthopedics Medicine. Radiology Overview of Arthritic Processes.
Mochizuki T, Ikari K, Okazaki K. Delayed Diagnosis of Psoriatic Arthritis Mutilans due to Arthritis Prior to Skin Lesion. Case Rep Rheumatol. 2018;2018:4216938. doi:10.1155/2018/4216938
Laasonen L, Gudbjornsson B, Ejstrup L, et al. Radiographic development during three decades in a patient with psoriatic arthritis mutilans. Acta Radiol Open. 2015;4(7):2058460115588098. doi:10.1177/2058460115588098
Ferreira MB, Sá N, Rocha SM, Marinho A. Opera glass hands: the phenotype of arthritis mutilans. Case Reports. 2013;2013:bcr2013200035. doi:10.1136/bcr-2013-200035
Center for Drug Evaluation and Research, U.S. Food and Drug Administration. Humira.
Nelson FRT, Blauvelt CT. The hand and wrist. In: A Manual of Orthopaedic Terminology. Elsevier; 2015:307-341. doi:10.1016/B978-0-323-22158-0.00010-X
Arthritis Foundation. Occupational Therapy for Arthritis.
Additional Reading
Aliu, O.; Nestcher, D.; and Peltier, M. Failure of Small Joint Arthrodesis from Resorption Around a Compression Screw in a Patient with Lupus-Associated Arthritis Mutilans: Case Report. Hand. 2008 Mar;3(1):72-5. doi:10.1007/s11552-007-9055-1
Bell, L.; Murphy, C.; Wynne, B. et al. Acute Presentation of Arthritis Mutilans. J Rheumatol. 2011 Jan;38 (1):174-5. doi:10.3899/jrheum.100579
Yin, Y.; Lui, S.; Xiao, H. et al. Opera-Glass Hand in a Patient with Rheumatoid Arthritis. J Clin Rheumatol. 2016 Jun; 22(4): 215. doi:10.1097/RHU.0000000000000388
By Lana Barhum
Lana Barhum has been a freelance medical writer since 2009. She shares advice on living well with chronic disease.






Post comments