
Many people enjoy kickstarting their day with the enticing aroma of coffee. The moment caffeine takes effect, it feels as if a fog has been lifted from the brain and our vision. Everything suddenly becomes crisp and bright.
Wakefulness and Sleep
Before you fully wake up, tiny caffeine molecules are already busy blocking adenosine from binding to its receptors in your brain. Cells rely on adenosine triphosphate (ATP) for energy metabolism, and adenosine is a byproduct of that process. As we stay active throughout the day, levels of adenosine accumulate in the brain and bind to adenosine receptors to promote sleep—essentially acting as an indicator of our “sleep debt” and stress. But when caffeine latches onto these receptors, adenosine can’t do its job, and you feel alert again.
Yet as the clock ticks past midnight, a new challenge arises for many: actually falling asleep. It’s not uncommon to lie awake thinking about the next day’s tasks during the hours meant for rest. In fact, nearly one-third of adults worldwide grapple with such sleep troubles. Fortunately, there are medications designed to help with this.
Beyond adenosine, another well-known sleep-related molecule is melatonin. When you switch off the lights at bedtime, the pineal gland in your brain releases melatonin in the dark environment. This lowers your core body temperature, nudges you into a calmer state, and helps induce sleepiness. Research has shown melatonin can ease occasional insomnia and assist with jet lag. Alongside related supplements, it’s also beneficial for people with delayed sleep phase syndrome—those whose sleep and wake times are consistently two to four hours later than the norm.
Another molecule with a profound impact on sleep is gamma-aminobutyric acid (GABA), an inhibitory neurotransmitter in the brain. By binding to GABA-A receptors, GABA reduces neuronal excitability, helping you relax and drift off. Many common sleep aids work by enhancing this inhibitory effect at GABA-A receptors, leading to reduced neuronal activity and, in turn, sleep.

Such medications include benzodiazepines, non-benzodiazepines (with zolpidem being the most common), and barbiturates. Although these drugs all target GABA-A receptors, they bind to different sites, meaning they can treat not only anxiety and insomnia but also serve other functions. Collectively, these medications belong to a broader group known as sedatives, whose exact effect—be it anti-anxiety, sedation, hypnosis, or anesthesia—depends on how they interact with GABA-A receptors. It’s important to be aware that these drugs are best used short-term and in low doses, as high doses can lead to coma, other severe consequences, and addiction.
Is Sleeping All It Takes for Quality Rest?
What exactly is the difference between dozing off under the influence of medication versus naturally drifting into slumber? Are the two equally beneficial? At least for some medications, the answer is no. For instance, zolpidem appears to disrupt certain natural processes in the brain during sleep.

In a recent study published in Cell, researchers investigated how the brain cleans itself during natural sleep—and found that zolpidem seems to interfere with this process. The paper’s corresponding author, Danish neuroscientist Maiken Nedergaard at the University of Rochester, named the “glymphatic system,” the brain’s own cleaning mechanism. In 2012 and 2013, her team published two studies demonstrating that during sleep, cerebrospinal fluid (CSF) flows into the interstitial spaces of the brain, facilitating waste removal. Eventually, the waste-laden CSF exits through aquaporin-4 (AQP4) channels on astrocytes. Nedergaard likens the process to turning on a “dishwasher” before bed, so that by morning, the brain is “clean.”
In their new study, Nedergaard and colleagues discovered the pivotal role of norepinephrine (noradrenaline) in cleansing the mouse brain. During sleep, the locus coeruleus in the brainstem—rich in norepinephrine-producing neurons—releases this neurotransmitter. By observing mice, the researchers confirmed that during deep sleep, norepinephrine’s effect on blood flow appears crucial for flushing out the brain’s internal waste.
Roughly every 50 seconds in deep sleep, the brainstem emits a pulse of norepinephrine. This causes blood vessels to constrict slightly and produce a slow, rhythmic pulsing. Those pulses help cerebrospinal fluid flow in a steady pattern, washing away accumulated debris.
However, when mice are given the sleep aid zolpidem, this cleaning process is noticeably disrupted. During deep sleep, mice on zolpidem have about 50% less norepinephrine release compared to mice that fall asleep naturally, which reduces CSF flow by over 30%. In other words, zolpidem somewhat hinders the brain’s waste clearance. Researchers have observed similar patterns of norepinephrine fluctuation, blood flow, and CSF movement in humans, suggesting that further study is needed to understand the full ramifications in people.
Which Sleep Stage Matters Most?
Most sleeping pills help people nod off more quickly. However, some seem to alter our sleep architecture. For example, benzodiazepines tend to increase lighter sleep and suppress deep sleep, potentially affecting sleep quality. One earlier study found zolpidem might improve sleep quality by boosting slow-wave sleep (also called non-rapid eye movement, or NREM sleep), mainly in stages N2 and N3, while reducing nighttime awakenings. But based on recent findings, the story might be more nuanced.
After we fall asleep, the brain cycles through roughly four to six sleep cycles, each containing three stages of slow-wave sleep (SWS) followed by a rapid eye movement (REM) stage.
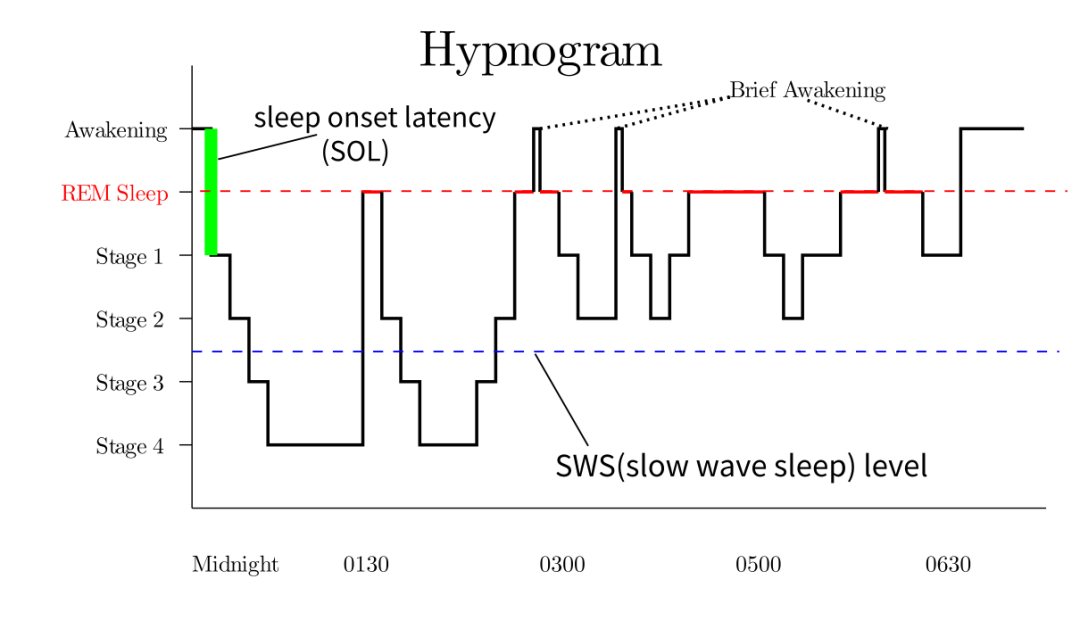
Sleep Phase Diagram Series——Wikipedia
Among these stages, research often points to N3 (deep sleep) and REM as especially important. Deep sleep is considered “restorative”: Heart rate and respiration reach their lowest point, making it hard to wake up. And even if you are awakened during this stage, you may need an hour or two to feel fully alert. Adults typically spend about 20–25% of total sleep time in deep sleep, which is critical for physical recovery, cell growth, and immune function. Even though brain activity slows down during deep sleep, evidence suggests it enhances insight, creativity, and memory—possibly linked to increased CSF flow and waste clearance in the brain.
Over the course of a night, however, time spent in N3 gradually declines while REM periods lengthen. REM is also the stage in which most dreaming occurs. Research has shown that chronic REM deprivation can be lethal for lab animals; if they are infected and then deprived of REM sleep, their survival rates plummet. Though these studies are somewhat grim, they underline the likely essential role REM plays.
One well-established conclusion is that REM helps consolidate various types of memories while pruning weaker “noise-like” traces. It also enables the brain to integrate new information, re-evaluate the day’s stressors and emotional responses, and regulate mood.

Interestingly, the reason people so often fail to recall their dreams is also linked to norepinephrine. During the day, norepinephrine release helps maintain wakefulness and focus, which is crucial for forming new memories. But at night, particularly in REM sleep, neurons in the locus coeruleus are almost silent, releasing very little norepinephrine. Consequently, the hippocampus and amygdala can’t generate the synaptic plasticity needed for memory formation—meaning you typically don’t remember your vivid REM dreams.
So, while sleeping pills may help you fall asleep faster, research suggests they might impair the brain’s natural “cleanup crew.” As scientists continue to explore precisely how these medications affect sleep architecture and the glymphatic system, one thing is clear: there’s more to quality sleep than simply lying unconscious through the night. The best rest is the kind that not only helps us feel refreshed when we wake up but also allows the brain to tidy up while we’re blissfully unaware.






Post comments