by Stephanie Baum , Medical Xpress
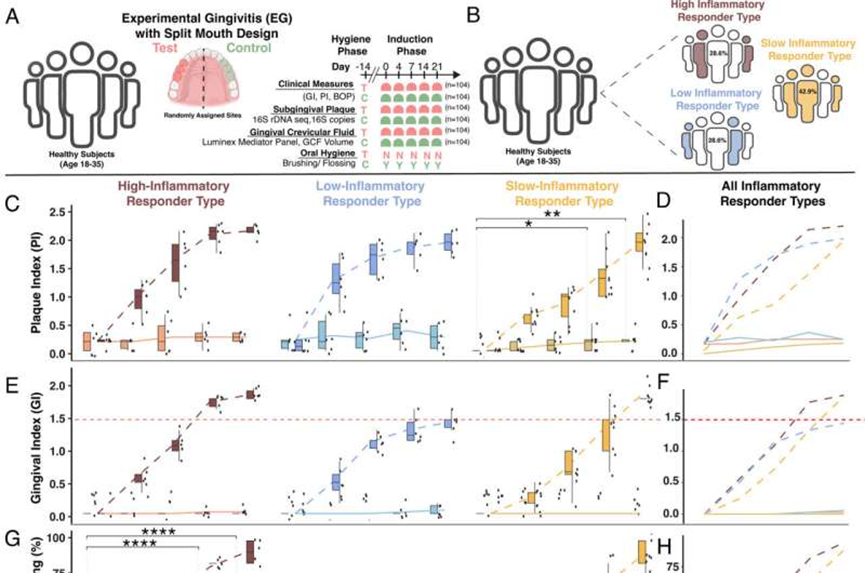
EG incorporating a split mouth design reveals control sites are not static and vary by IRT. (A) Study overview highlighting the clinical EG model. (B) Proportion of clinical IRTs (Materials and Methods). (C) PI stratified by IRT test and control sites during the Induction phase (Days 0 to 21). (D) Mean PI by IRT test and control sites during the Induction phase. (E) GI stratified by IRT test and control sites during the Induction phase. Red dashed line represents a GI value of 1.5 and represents the difference between high and low levels of clinically observed inflammation. (F) Mean GI by IRT test and control sites during the Induction phase. (G) BOP stratified by IRT test and control sites during the Induction phase. (H) Mean BOP by IRT test and control sites during the Induction phase. (I) GCF volume stratified by IRT test and control sites during the Induction phase. (J) Mean GCF volume by IRT test and control sites during the Induction phase. (K) Bacterial Load (16S rRNA gene copies) stratified by IRT test and control sites during the Induction phase. (L) Mean Bacterial Load by IRT test and control sites during the Induction phase. Significance level indicated by asterisks: *P < 0.05, **P ≤ 0.01, ***P ≤ 0.001, and ****P ≤ 0.0001. All significance test results between test and control sites provided in SI Appendix,Tables S6–S11 and Figs. S1 and S2. Credit: Proceedings of the National Academy of Sciences (2023). DOI: 10.1073/pnas.2306020120
Much evidence exists to show that in humans, oral inflammatory conditions such as periodontal disease can affect overall health. In its later stages, periodontal disease can lead to systemic issues such as cancer, cardiovascular disease, and diabetes. Until now, however, little has been known about how it might affect healthy oral tissue.
To guard against periodontal disease, dentists and hygienists typically advise regular thorough flossing and tooth brushing as key parts of oral hygiene maintenance. However, new research shows that localized gingivitis—the first stage of periodontal disease—can induce changes in the oral microbiome and can lead to immune responses in distant healthy parts of the mouth. Furthermore, the timing and intensity of such responses can vary among individuals.
A new study, by researchers from the University of Washington, Rutgers University, King Abdulaziz University, and the Department of Oral Health Research at the Colgate Palmolive Company, is titled "Localized microbially induced inflammation influences distant healthy tissues in the human oral cavity." It is published in Proceedings of the National Academy of Sciences.
Existing research shows that humans can exhibit different immune responses to bacterial and viral pathogens. Within the mouth, differing immune responses to microbial invasion have been similarly observed. In this study, the researchers sought to observe and describe contrasts in microbial gingival inflammation induced in study subjects.
The research involved 21 adults between the ages of 18 and 35 in good general health. Fourteen days before the experimental phase began, each volunteer received a professional teeth cleaning to establish normal oral health.
As this was a split-mouth design study, two weeks later (on study day 0), each subject received a personalized acrylic intraoral stent to cover a randomly assigned test site of three teeth on the upper maxilla (either #3, 4, and 5 or #12, 13, and 14). The three teeth located contralateral to each test site were considered the control site.
For the next 21 days, the test subjects covered the test sites with their stents while they maintained regular oral hygiene and brushed the rest of their teeth with toothpaste containing fluoride. During this three-week period, the researchers induced gingival inflammation, taking gingival samples on days 0, 4, 7, 14, and 21, and noting the timing of the amounts and types of oral bacteria and bleeding on probing observed in each volunteer.
As the study proceeded, the healthy control sites (on which the volunteers maintained regular oral hygiene) exhibited indicators of gingival inflammation similar to those seen in the test sites, but which developed to a lesser extent and at a slower pace.
Interestingly, based on the test subjects' bacterial responses, the researchers were able to categorize each as one of three inflammatory responder types (IRTs): high-IRT, low-IRT, or slow-IRT. High-IRTs and slow-IRTs exhibited more vulnerability than low-IRTs to high inflammation, with longer development periods of bacterial loads in slow-IRTs. The IRT groups did not reflect notable differences in sex and age.
These results are important because they add to existing knowledge of how inflammation in a localized area can ultimately affect healthy tissues in a distant area and possibly lead to infection. Moreover, despite maintaining oral hygiene, each study subject developed varying levels of oral inflammation at different rates according to their specific inflammatory responder type.
Crucially, what isn't clear is what determines an individual's inflammatory responder type. This suggests that while maintaining one's oral hygiene through daily brushing and flossing is essential, it is only one component of a comprehensive dental health scheme. Regular hygiene visits and dental checkups are still necessary to detect any distant inflammation.






Post comments