Mixed reality (mixed reality, MR) is the application of computers to generate virtual images from imaging data and superimpose them with the real scene on the spot, realizing the interaction between virtual and real scenes.
Existing optical navigation results in neurosurgery are usually flat images in the monitor, and even 3D reconstructed images are displayed as downscaled 2D images, which need to be transformed into 3D positional relationships in the operator's mind and correspond to the patient's real anatomical position, which relies on the operator's rich anatomical knowledge and surgical experience. If the angle of the surgical bed is adjusted according to the body position, or the angle of the surgical approach is adjusted during the operation, and the angle and position of the lesion change accordingly, the surgeon is required to reconstruct the relative anatomical position of the patient in his/her mind. This requires repeated training over a long period of time and may have the disadvantage of not being standardized and not easy to learn and master. Conventional navigation requires the operator to shift his/her vision from the surgical area to the monitor, which lengthens the surgical time and increases the risk of surgery by shifting the vision back and forth. Mixed reality technology can visualize the patient's lesion by generating virtual images and projecting them into the surgical reality environment. Neurosurgery can directly visualize the lesion, scalp, skull, nerve fiber bundles, ventricles, blood vessels and other structures in three dimensions by applying MR technology, and intraoperative navigation can be carried out by measuring the distance between the lesion and the anatomical markers.
The Department of Neurosurgery of the Second Affiliated Hospital of Chongqing Medical University applies mixed reality technology and uses holographic images and realistic surgery to integrate with each other during surgery, successfully completing the complex paracentral giant aneurysm clamping graduation, which makes the surgery more precise and minimally invasive.
01 Case Characteristics
The patient is a middle-aged female, 52 years old, admitted to the hospital with dizziness for 6 months.
Admission examination: she was conscious, answered questions tangentially, stepped into the hospital area, roughly measured bilateral visual acuity and visual field without obvious abnormality, bilateral pupil diameter of about 3mm, sensitive to light reflex, bilateral eye movement was normal, limb muscle strength was normal, pathological reflexes were not elicited;
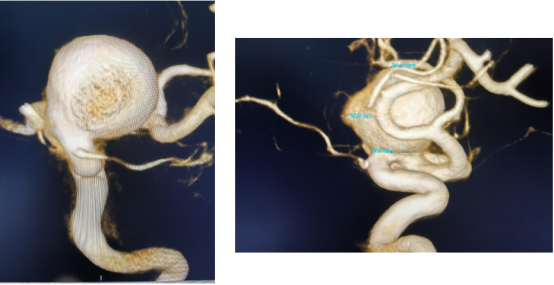
CTA of the head in our hospital showed: left internal carotid artery paracentral aneurysm;
After admission, complete visual acuity, visual field examination, pituitary function hormones, sex hormones, cortisol and thyroid function were not abnormal;
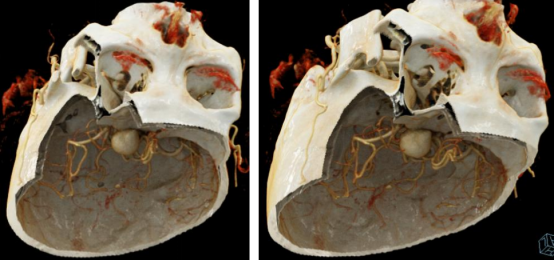
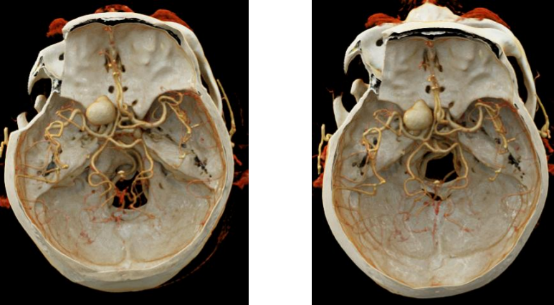
CTA of the head in our hospital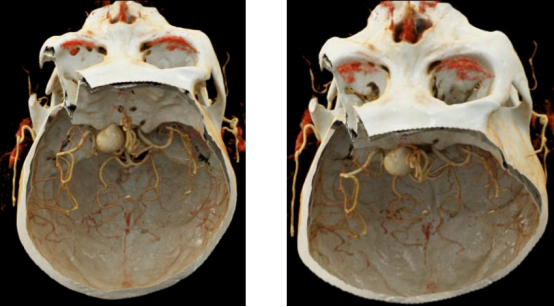
Our DSA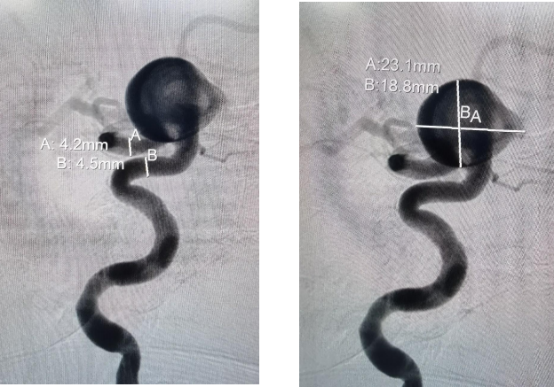
High Resolution MR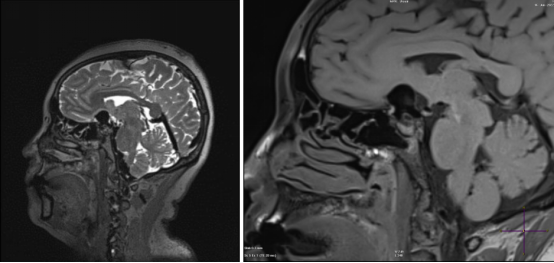
VR reconstruction of our hospital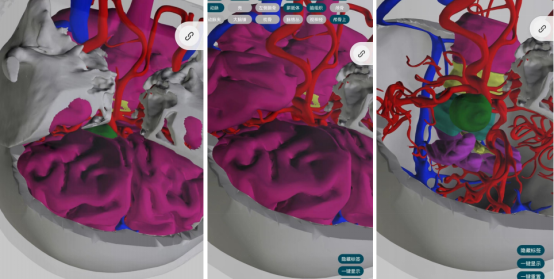
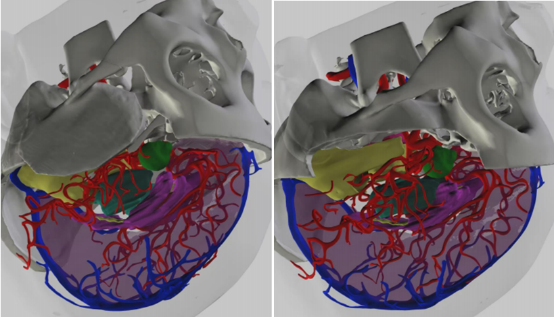
Based on the preoperative VR reconstruction, it is possible to determine the extent of bone resection to expose the aneurysm neck, reducing the need for unnecessary intraoperative bone obliteration and making the procedure more precise.
02 Treatment Options
Temporary cervical block + epidural abrasion of the pterygoid ridge, part of the pterygoid wing, anterior bed protrusion. The aneurysm is clamped behind the pterygoid winglets (opening the distal ring of the internal carotid artery if necessary).
03 Surgical procedure


During the operation, Dr. Liu's team applied high-tech means such as mixed reality and intraoperative neurophysiological monitoring to realize the fusion of holographic images in the operating room and the reality of the surgery, to locate the site of the aneurysm under the "fluoroscopy" before the operation and to clarify the exposure of the aneurysm at different angles and its adjacency with the surrounding nerves, brain tissues and blood vessels.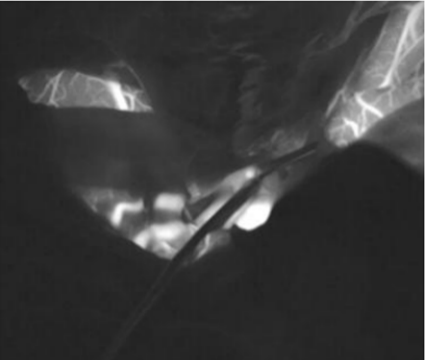
Figure 1 | Pre-clamping image showing the beginning of the ophthalmic artery and the aneurysm highlights.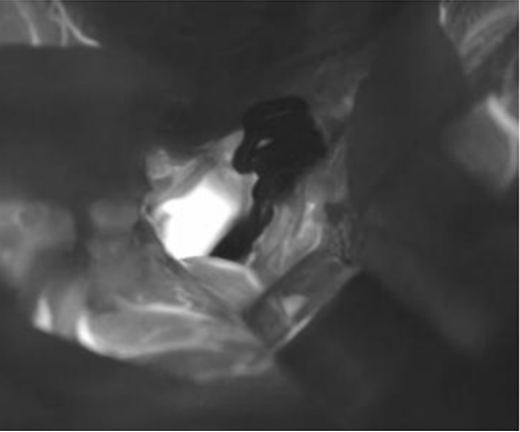
Figure 2 | Post-clamping image shows that the aneurysm is not visible and the aneurysm-carrying artery is patent without stenosis.
04 Postoperative results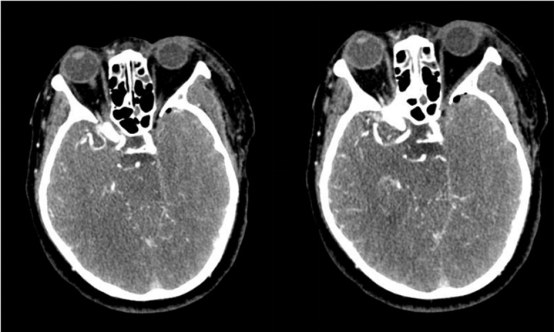
Figure 3 | The patient's left anterior bed protrusion, pterygoid winglet and part of the pterygoid winglet have been abraded.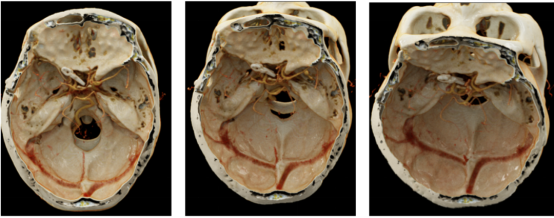
Fig. 4 | The resection area of the bone window is consistent with the preoperative and intraoperative planning.
The application of mixed reality technology gives neurosurgeons a more intuitive and clearer view of anatomical relationships, pushing the concept of minimally invasive and precise neurosurgery to a whole new level, and may revolutionize the way neurosurgery is planned and performed in the future.
Neurosurgery-Mixed Reality








Post comments