What You Should Eat and What You Should Avoid When You Have Liver Disease
By Charles Daniel
Medically reviewed by Robert Burakoff, MD
A cirrhosis diet is designed to help people with cirrhosis who may become malnourished due to changes in their metabolism and digestion that occur as the liver becomes more damaged.
When you have cirrhosis, what you eat and drink each day is especially important. Many foods to avoid with cirrhosis contain protein, sodium, and sugar that require your liver to work harder—a demand it may no longer be able to meet.
This article explains how a cirrhosis diet plan may be crafted with the help of your healthcare team members, such as a registered dietitian. This will ensure that you're adequately nourished and avoid choices that can worsen your condition and otherwise impact your health.
What Is Cirrhosis?
Cirrhosis is scarring of the liver. Scar tissue forms because of injury or long-term disease.1 Scar tissue is a tough, fibrous tissue made of collagen. Scarring blocks the flow of blood and oxygen through your liver tissues.
The liver has more than 500 functions, making it one of the most vital organs.2 If your liver is damaged from cirrhosis, it is not able to do what a healthy liver does—make protein, help fight infections, clean the blood, help digest food, and store energy.1
Benefits of the Cirrhosis Diet
A cirrhosis diet can help provide adequate nutrition, reduce the amount of work your liver needs to do, thwart related complications, and prevent further liver damage.
Research has shown that people with liver disease who aren't adequately nourished are more likely to experience complications from cirrhosis, including death.3
Authors of a 2018 article in the Journal of Clinical Gastroenterology note that "dietary management of cirrhosis is not a one-size-fits-all approach." A cirrhosis diet should be started early in treatment to improve the prognosis and outcomes.4
Unfortunately, existing scarring from cirrhosis cannot be reversed. Diet, then, is a key way to minimize complications and keep it from getting worse.
A Complete Guide to a Low-Protein Diet
How the Cirrhosis Diet Works
Your cirrhosis diet will need to be tailored based on your overall health and individual needs, but there are some general dietary guidelines that often shape this eating plan:5
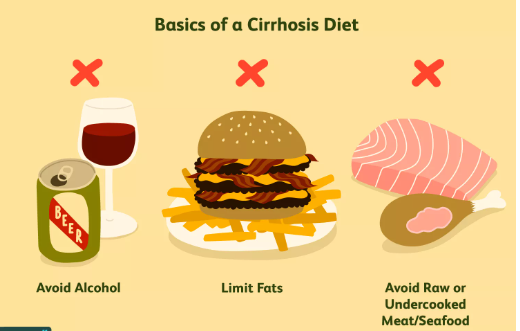
Avoiding alcohol: Any amount of alcohol is considered unsafe for people with cirrhosis, as it's a potential cause of more liver damage—even liver failure. Drinking can also contribute to malnutrition and other health concerns.
Limiting fats: The body digests fats using bile, a yellow-green fluid made in the liver. When the liver is damaged, the production and supply of bile may be affected, leading to digestive symptoms. A liver that isn’t working well has a hard time processing a high-fat meal. (Healthy fats can be included in moderation.)
Avoiding raw or undercooked meat and seafood: People with liver damage from cirrhosis have impaired immune function, so bacteria and viruses that these foods can harbor can lead to a potentially serious infection.
In addition to changing the content of your diet, you may need to change the quantity of the food you eat. Having liver disease can increase your risk for malnourishment, so you may need to eat more calories in a day to meet the increased energy demands on your body.6
If you have liver disease, know that the recommendations for protein intake vary. The influence of protein on liver disease is somewhat controversial and still being studied.7
You'll need to consult with your healthcare provider or a registered dietitian to determine the exact amount of protein recommended for you. The calories from protein will be an essential component of a varied and nutritious diet, and protein is key to preventing muscle atrophy (thinning).8
Your healthcare provider may want you to make additional, specific changes to your diet to help manage or prevent other conditions people with liver cirrhosis may be more likely to get.
Duration
If you are at risk for liver disease, your healthcare provider may want you to follow a cirrhosis diet even if you don’t feel sick. Someone in the early stages of liver disease (compensated phase) usually doesn’t have any symptoms.
Signs of liver disease may take years to show up, and they do so only once damage to the liver has become severe (decompensated phase).9 Since changing how you eat can only help to prevent additional liver damage, but can’t heal what’s already occurred, you will likely need to be on a cirrhosis diet plan for a long time.
What to Eat and Not Eat
If you’re following a cirrhosis diet, there are some foods and beverages you’ll need to strictly avoid. However, you’ll have your choice of many nutritious and tasty foods, including fresh produce, whole grains, and plant-based protein.
Foods to Eat
Fruits and vegetables (raw or cooked without butter, oil, or salt)
Eggs, egg whites
Cooked fish (salmon, tuna)
Lean chicken or turkey (without the skin)
Low-fat Greek yogurt
Cream cheese, ricotta
Low-fat cheese (low-sodium cottage cheese, fresh mozzarella)
Nuts and seeds (unsalted)
Dried beans and legumes
Nut butters (unsalted)
Tofu
Fortified milk alternatives (almond, soy, rice)
Margarine
Oats
Whole grain bread, crackers, and cereals
Brown rice
Olive oil
Fresh herbs
Low-fat milk
Garlic
Ginger
Quinoa, couscous, pasta, rice
Granola and cereal bars
Coconut water
Meal/nutritional supplements, as approved
Foods to Avoid
Raw or partially raw fish and shellfish (e.g., oysters, clams)
Fast food, fried food
Red meat
Canned food (meat, soup, vegetables)
Packaged, processed snacks and meals (incl. frozen)
Hot dogs, sausage, lunchmeat
Sauerkraut, pickles
Buttermilk
Tomato sauce or paste
Instant hot cereal or oatmeal
Potato chips, pretzels, rice cakes, crackers, popcorn
Refined white flour pasta, bread, and white rice
Oils high in trans fat or partially hydrogenated oils (palm oil, coconut oil)
Breading, coating, and stuffing mixes
Full-fat dairy products
Bread, biscuit, pancake, and baked good mixes
Pastries, cake, cookies, muffins, doughnuts
American, Parmesan, Swiss, blue, feta, cottage cheese, cheese slices or spreads
Pudding, custard, or frosting mixes
Table salt, sea salt, mixed seasonings
Ketchup, soy sauce, salsa, salad dressing, steak sauce
Bouillon cubes, broth, gravy, and stock
Caffeinated tea, coffee, and soft drinks
Alcohol
Fruits and vegetables: Choose fresh produce when possible, as canned varieties usually have sodium and sugar. Fruits high in polyphenols (a type of antioxidant) have been shown to protect liver health.10
Blueberries, strawberries, pomegranates, and grapes are fruits with these benefits. Many herbs and vegetables are high in polyphenols too. Add fruit to cereal or oats for extra nutrition, fiber, and a little natural sweetness. Fiber-rich fruits like apples make a healthy and satisfying snack on their own.
Dairy: Full-fat dairy products will likely be too hard for your body to digest. Stick to low-fat Greek yogurt, small portions of low-sodium hard cheese, and fortified dairy-free milk alternatives like almond or soy.
Rich, milk-based desserts like pudding, custard, and ice cream should be limited. You may need to avoid them completely on a cirrhosis diet if you have significant trouble processing fat and sugar.
Grains: Choose whole-grain bread, pasta, brown rice, and cereal instead of those made with refined white flour. Granola and granola bars may be approved for quick snacks as long as they’re low in sugar and sodium.
Protein: Red meat isn’t approved for a cirrhosis diet, nor is any kind of processed lunch meat or sausage. Small servings of lean poultry without the skin, some types of fresh-caught fish (such as salmon), and eggs or egg whites may be suitable.
Most of your protein should come from plant-based sources such as dried beans and legumes, small portions of unsalted nuts or nut butter, and tofu.
Desserts: Packaged cake, cookie, brownie, biscuit, pancake, and waffle mixes can be high in sugar and salt, so it's best to avoid them. In general, avoid pastries, doughnuts, and muffins, unless you can make your own low-fat, low-sugar, and low-salt versions.
Beverages: You cannot drink alcohol if you have liver cirrhosis, but there are other beverage options. Water is the most hydrating choice, but if you are on a low-sodium diet, check the labels on bottled water as some contain sodium. Milk and juice should only be consumed if pasteurized.
While some research has suggested coffee (but not other caffeine-containing beverages) could have benefits for people with alcohol-related liver disease, most medical professionals advise that patients with cirrhosis avoid caffeinated beverages, including coffee, tea, and soft drinks.
Supplements: Vitamins with antioxidant properties, like vitamins C and E, may help to promote liver health. Vitamin D is essential to overall health, especially in preventing non-alcoholic fatty liver disease. Keep in mind that some vitamins (or too much of them) can be toxic to a damaged liver; always talk to a healthcare provider before taking any dietary supplements.11
When to Eat
Liver disease can lead to malnourishment, in which case your healthcare provider might want you to eat more calories.12 If you don’t feel up to eating larger meals to increase your caloric intake, try eating small, frequent meals and snacks throughout the day.
Some people with liver disease find they wake up in the night. They may stay awake for long stretches and end up taking naps during the day. If you are awake in the middle of the night, research has shown that having a late-night snack can be helpful for people with cirrhosis.
A healthy late-night snack could include:
Low-fat Greek yogurt with berries and a few nuts sprinkled on top
A bowl of whole-grain cereal with soy or almond milk and fruit
If your sleep schedule is interrupted, be sure to plan your meals around when you are awake, whether it’s during the day or at night. Try to eat a meal or snack every couple of hours.
Cooking Tips
Try grilling or boiling veggies and preparing them without oil or butter.
If you’re reducing your sodium intake as part of a cirrhosis diet, try using fresh herbs and spices instead of table salt. If you’re used to adding salt to your food and find it difficult to break the habit, your healthcare provider may suggest using a salt substitute.
When cooking meat, start by choosing lean cuts. Skinless poultry is a healthier option than red meat.
You may be allowed to have small portions of beef on occasion depending on how it’s prepared. For example, grilling meat instead of frying with oil or butter reduces the fat content and prevents it from becoming too greasy for a cirrhosis diet.
In addition to avoiding raw or partially cooked meat and seafood, practice proper food handling and safety practices to further reduce your risk of foodborne infections.
Modifications
You may need to adapt your diet if you develop complications from cirrhosis, such as ascites, hypoglycemia, and encephalopathy.13 If you develop one or more of these conditions, your healthcare provider may recommend additional changes to your diet, including limiting salt, sugar, and protein.
Fluid Retention
Two types of fluid retention can occur when people have cirrhosis: ascites and edema.
Ascites is the accumulation of large amounts of fluid in the abdomen.14 Edema is swelling caused by fluid in your body's tissues. It usually occurs in the feet, ankles, and legs, but it can involve your entire body.15
Healthcare providers usually require a strict no-salt diet for people who have cirrhosis with ascites or edema, as sodium can make the condition worse.16
The daily recommended sodium intake for people with ascites is 88 millimoles per liter (mmol) per day.16 The typical American diet contains 200 to 300 mmol per liter of sodium per day.
Prepackaged and convenience food items are often high in sodium or contain added salt. If you're not routinely checking the nutrition labels, you may not be aware of how much sodium you’re consuming.
When you’re grocery shopping, a good rule of thumb is to focus on what you can buy along the perimeter of the store—fresh produce, lean meats, and low-fat dairy—which are low-sodium choices. Avoid the packaged snacks, cereals, and sodas found in the middle aisles.
High Blood Pressure
Your body carries blood to your liver through a large blood vessel called the portal vein. Cirrhosis slows your blood flow and puts stress on the portal vein. This causes high blood pressure known as portal hypertension.17
Along with medications to treat high blood pressure, your healthcare provider will usually recommend a low-sodium diet,
Encephalopathy
As the body digests protein, it creates a byproduct called ammonia. When the liver is functioning properly, ammonia is cleared without issue. But a damaged liver can't handle a normal amount of protein, let alone any extra.
The more protein the body tries to digest, the more ammonia can build up. At high levels, it becomes toxic to the brain and can cause memory problems, dementia-like symptoms, and a serious complication called encephalopathy.12
If you have cirrhosis, focus on including plant-based protein sources in your diet instead of meat. Your healthcare provider may give you a specific limit on how much protein you can have per meal or per day.
Hypoglycemia and Diabetes
Hypoglycemia, or low blood sugar, is another common problem associated with cirrhosis. When your liver is healthy it stores energy from the carbohydrates you eat in an easily accessible form called glycogen.
If you have cirrhosis, your liver isn’t able to store enough energy in the form of glycogen. As a result, people with liver disease may experience episodes of low blood sugar.
A little over 30% of people with cirrhosis also have diabetes, which can sometimes lead to hypoglycemia related to medications used to treat diabetes.1819
Research has shown that eating high-fiber meals with a low glycemic index can help manage hypoglycemia and diabetes in people with cirrhosis.
Considerations
It's important to stick with your cirrhosis diet to prevent further liver damage. You can do this by following some general principles to help set yourself up for success.
General nutrition is important and healthy foods are part of a cirrhosis diet. Your healthcare provider may have you take vitamins or nutritional supplements, though, because your condition makes it harder to stay nourished. That's especially true if you have nausea or gastrointestinal (GI) symptoms.
Supplements or multivitamins that contain a lot of vitamin A can be toxic to the liver.20 Iron can be hard for the liver to process in high doses. Talk with your healthcare provider about any vitamin or supplement products, which can interact with medications or cause GI symptoms.
Changes in your diet are critical, so you should approach the cirrhosis diet as a positive lifestyle decision to promote your health. That means reading labels for fat, sugar, and salt at the grocery store so that you'll know you're making the best possible choices. Specific situations may include:
Selecting gluten-free bread, pasta, and crackers if you also have celiac disease
Limiting pasta made from beans and legumes that are high in protein for a cirrhosis diet
Reducing protein from nuts, seeds, and tofu if you follow a plant-based diet
Fresh produce, dried beans, and other ingredients you need to make healthy cirrhosis diet recipes can be affordable with careful planning and shopping. It will help you make the most of your budget while avoiding foods that can worsen cirrhosis.
Keep in mind that your cirrhosis diet plan also includes meals when you eat out. Don't hesitate to ask about your menu options when dining at restaurants.
Your healthcare provider, as well as a registered dietitian or nutritionist, can help you adjust a cirrhosis diet plan to fit your needs.
Your success in sticking to a cirrhosis diet plan also will depend on support from family members and friends. This is especially true if you may need help with meal prep and planning due to advanced liver disease.
While your healthcare team is the primary source for information about your cirrhosis diet, you may wish to consider a support group in your area for people with liver disease. You can also look online for message boards, social media hashtags, or blogs where people share stories, experiences, and cirrhosis diet menu ideas.
If your healthcare provider wants you to take nutritional supplements or add drinks like Ensure to your diet, know that these can be expensive. If you have health insurance, ask if these supplements can be prescribed for you. If so, all or part of the cost of certain supplemental nutrition may be covered.
Summary
If you have cirrhosis, staying adequately nourished can be challenging. You may need to eat more or less of certain foods to ensure your body is getting the energy it needs.
It's also important that you pay close attention to your diet so you can avoid more damage to your liver. For example, you'll need to avoid alcohol, high-fat foods, and raw or partially cooked shellfish.
While changing the way you eat can't cure a liver that is already scarred, it can improve your quality of life and help prevent complications.
Talk with your healthcare provider or registered dietitian for nutrition recommendations tailored to your specific needs.
Sources
Medline Plus. Cirrhosis.
Bhatia SN, Underhill GH, Zaret KS, Fox IJ. Cell and tissue engineering for liver disease. Sci Transl Med. 2014;6(245):245sr2. doi:10.1126/scitranslmed.3005975
Bémeur C, Butterworth RF. Nutrition in the Management of Cirrhosis and its Neurological Complications. Journal of Clinical and Experimental Hepatology. 2014;4(2):141-150. doi:10.1016/j.jceh.2013.05.008
Yao C, Fung J, Chu N, Tan V. Dietary Interventions in Liver Cirrhosis. J Clin Gastroenterol. 2018;52(8):663-673. doi:10.1097/mcg.0000000000001071
National Institute of Diabetes and Digestive and Kidney Diseases. Eating, Diet, & Nutrition for Cirrhosis.
Purnak T, Yilmaz Y. Liver disease and malnutrition. Best Practice & Research Clinical Gastroenterology. 2013;27(4):619-629. doi:10.1016/j.bpg.2013.06.018
Barnard, Neal D., editor. Cirrhosis. Nutrition Guide for Clinicians, 3rd ed., Physicians Committee for Responsible Medicine, 2017.
McClain CJ. Nutrition in Patients With Cirrhosis. Gastroenterology & hepatology. 2016;12(8):507-510.
Angeli P, Bernardi M, Villanueva C, et al. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. Journal of Hepatology. 2018;69(2):406-460. doi:10.1016/j.jhep.2018.03.024
He K, Li Y, Guo X, Zhong L, Tang S. Food groups and the likelihood of non-alcoholic fatty liver disease: a systematic review and meta-analysis. Br J Nutr. 2020 Mar 6;124(1):1-13. doi: 10.1017/S0007114520000914
Jeznach-Steinhagen A, Ostrowska J, Czerwonogrodzka-Senczyna A, Boniecka I, Shahnazaryan U, Kuryłowicz A. Dietary and Pharmacological Treatment of Nonalcoholic Fatty Liver Disease. Medicina (Kaunas). 2019 May 20;55(5):166. doi:10.3390/medicina55050166.
U.S. Department of Veterans Affairs. Eating tips for people with cirrhosis.
Volk M. Liver cirrhosis: a toolkit for patients. University of Michigan Health System.
Medline Plus. Ascites.
Medline Plus. Edema.
Johns Hopkins Medicine. Ascites.
American Academy of Family Physicians. Cirrhosis and portal hypertension.
Hamed AE, Elsahar M, Elwan NM, et al. Managing diabetes and liver disease association. Arab J Gastroenterol. 2018 Dec;19(4):166-179. doi: 10.1016/j.ajg.2018.08.003
Lee WG, Wells CI, McCall JL, Murphy R, Plank LD. Prevalence of diabetes in liver cirrhosis: A systematic review and meta-analysis. Diabetes Metab Res Rev. 2019 Sep;35(6):e3157. doi: 10.1002/dmrr.3157
National Institute of Health. LiverTox: Vitamin A.
By Charles Daniel
Charles Daniel, MPH, CHES is an infectious disease epidemiologist, specializing in hepatitis.






Post comments