In the fields of cardiac surgery and critical care medicine, extracorporeal life support (ECLS) has become a vital treatment modality for critically ill patients, particularly those following cardiac surgery, as well as those in cardiogenic shock, acute heart failure, and cardiac arrest. ECLS provides short-term circulatory support to patients who are unable to restore cardiac function, significantly improving survival rates. Despite its success in saving lives, ECLS is associated with significant complications, particularly neurological ones, which remain a major challenge in clinical practice. These complications not only hinder postoperative recovery but can also lead to long-term cognitive impairments and a reduced quality of life. Previous studies have suggested that ECLS-related neurological damage may be linked to several factors, including changes in brain perfusion, hemodynamic disturbances, underlying comorbidities, and vascular conditions. However, despite the availability of various cannulation strategies—such as aortic, subclavian/axillary, and femoral cannulation—there remains a lack of systematic, quantitative comparative studies assessing the impact of different cannulation sites on neurological complications.
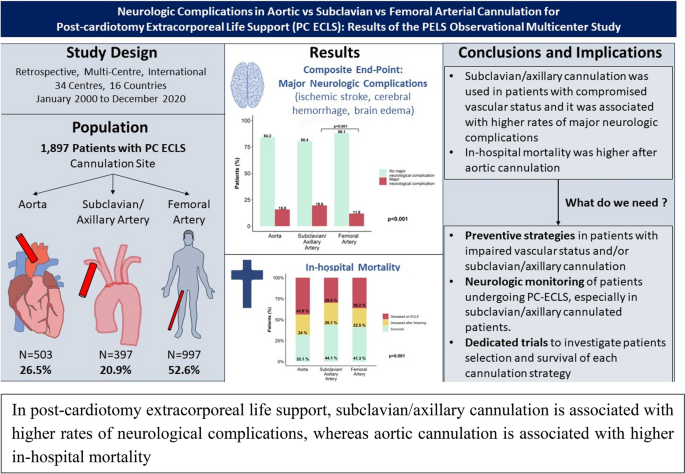
To address this gap, Chiarini et al. conducted a multicenter retrospective analysis involving 1,897 patients who received ECLS treatment between 2000 and 2020. Patients were grouped according to the cannulation site: aortic (26.5%), subclavian/axillary (20.9%), and femoral (52.6%). The primary endpoint of the study was the occurrence of composite neurological complications, including ischemic stroke, cerebral hemorrhage, and cerebral edema. Secondary endpoints included seizures, all-cause in-hospital mortality, and mortality related to neurological complications. Data were analyzed using a multivariable mixed-effects model, which controlled for potential confounding factors, to systematically evaluate the relationship between different cannulation methods and neurological complications.
The study results indicate that the incidence of composite neurological complications in the subclavian/axillary group was 19.6%, significantly higher than that in the femoral group (11.9%) and the aortic group (15.8%). The incidence of ischemic stroke in the subclavian/axillary group was 15.9%, markedly higher than in the femoral group (8.1%) and the aortic group (11.8%). The incidence of cerebral hemorrhage in the subclavian/axillary group was 5.9%, substantially higher than in the femoral group (2.3%) and the aortic group (3.2%). The incidence of seizures in the subclavian/axillary group was 3.4%, higher than in the aortic group (1.8%) and the femoral group (1.3%). These findings suggest that subclavian/axillary cannulation is associated with a higher incidence of neurological complications, particularly ischemic strokes and cerebral hemorrhages, potentially due to its adverse effects on brain perfusion, which may increase the risk of neurological damage.
Additionally, the in-hospital mortality rate was significantly higher in the aortic group (68.4%) compared to the subclavian/axillary group (56.2%) and the femoral group (58.9%). Although the aortic group exhibited a lower incidence of neurological complications, its higher mortality rate may be attributed to the more complex baseline conditions of the patients, such as preoperative cardiac arrest and emergency surgery. This finding underscores that the choice of cannulation strategy is not only linked to neurological outcomes but also closely associated with the patient's overall prognosis. It emphasizes the importance of considering individual clinical characteristics when selecting the optimal treatment strategy.
The study also highlighted that, despite the use of neuro-monitoring techniques in clinical practice, the utilization rate of neuro-monitoring in this study was relatively low, particularly among patients in the subclavian/axillary group. Inadequate neuro-monitoring may delay the recognition and intervention of neurological damage, potentially exacerbating the injury. Consequently, the study underscores the need to enhance neuro-monitoring, especially for high-risk patients. Early detection of neurological damage and prompt intervention could significantly improve patient outcomes.
In comparison to previous studies, this research employed a large-scale, multicenter retrospective design, increasing the generalizability of the findings and better reflecting the practice variations across different clinical settings. Moreover, this study is the first to systematically compare the impact of three different cannulation strategies on neurological complications, thus addressing a gap in the existing literature and providing valuable guidance for clinical decision-making. Additionally, the study emphasizes the importance of neuro-monitoring and suggests a more refined monitoring strategy for future research.
However, the study has several limitations, including the inherent constraints of its design, lack of long-term follow-up data, incomplete control of confounding factors, and insufficient neuro-monitoring. Future research should prioritize prospective randomized controlled trials, leveraging advanced technologies and multidisciplinary approaches to develop more precise and personalized treatment strategies for ECLS patients, ultimately aiming to improve survival rates and quality of life.
REFERENCES:Chiarini G, Mariani S, Schaefer A K, et al. Neurologic complications in patients receiving aortic versus subclavian versus femoral arterial cannulation for post-cardiotomy extracorporeal life support: results of the PELS observational multicenter study[J]. Critical Care, 2024, 28(1): 265.






Post comments