From: Conservative or liberal oxygen targets in patients on venoarterial extracorporeal membrane oxygenation
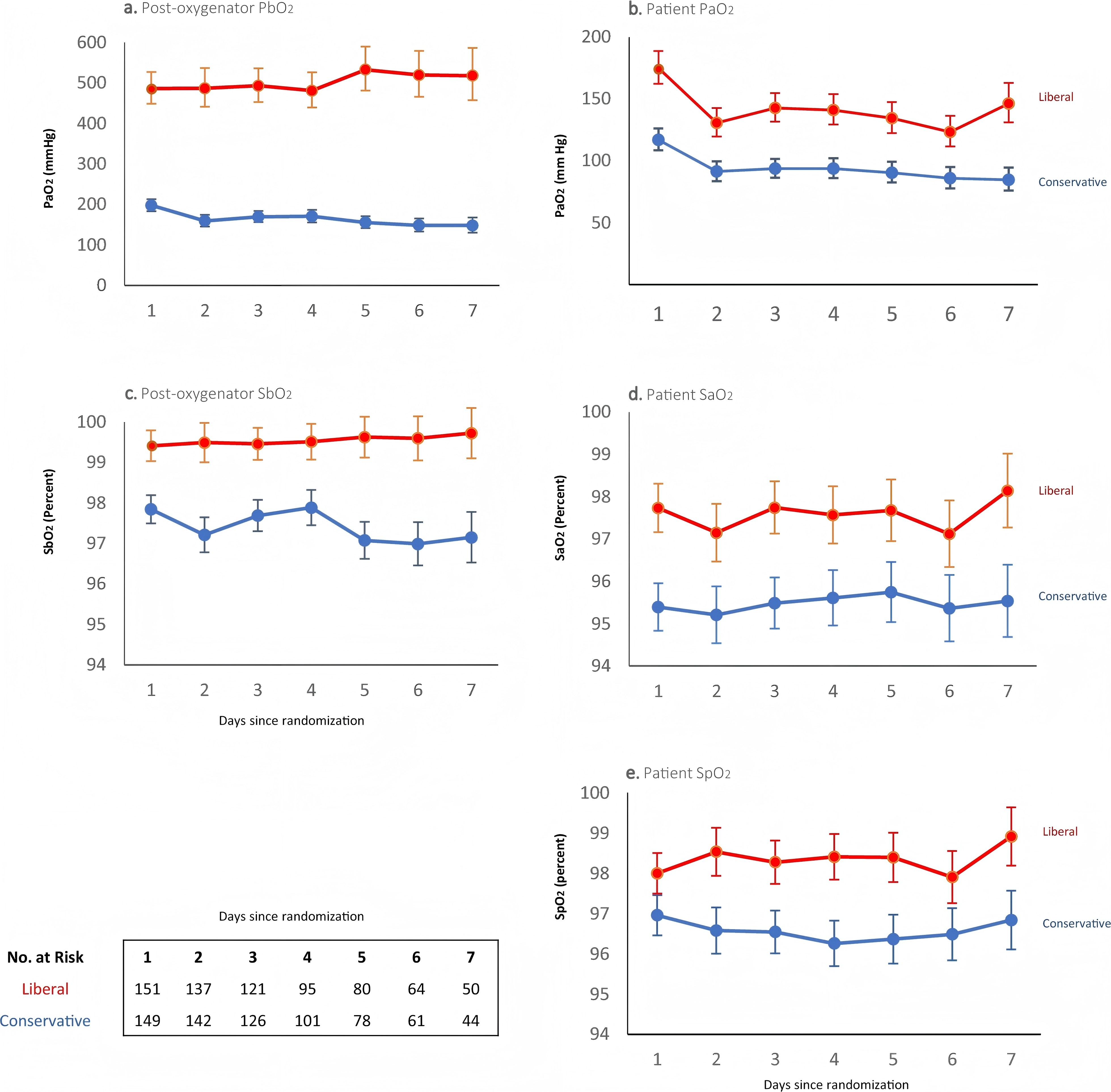
Partial pressures of arterial oxygen and oxygen saturations of the patient and post-oxygenator. Shown are the partial pressures (panels a., b.) and saturations (panels c.–e.) of oxygen recorded from the post-oxygenator (PbO2, SbO2), the radial arterial line (PaO2, SaO2) and pulse oximetry on the right hand (SpO2) of patients still on ECMO from day 1 to 7. Patients were assigned to either a conservative oxygen strategy (SaO2 92–96%) or to a liberal oxygen strategy (SaO2 97–100%) at the time of randomization. The intervention strategy was continued until cessation of ECMO. One patient in the conservative group who died on day 1, had no blood gas values recorded. All curves show the geometric mean and 95% confidence interval of the available values
Veno-arterial extracorporeal membrane oxygenation (VA-ECMO) is a clinical intervention commonly used to treat critically ill patients suffering from cardiogenic shock and acute cardiac arrest. One of the key challenges during VA-ECMO therapy is maintaining optimal oxygenation levels. Traditionally, hyperoxemia has been thought to help prevent hypoxemia and subsequent organ hypoxia. However, accumulating evidence now suggests that excessive oxygen levels may induce oxidative stress, leading to cellular injury, endothelial dysfunction, and inflammatory responses, which can worsen disease progression and contribute to long-term functional impairments. On the other hand, hypoxemia can result in inadequate tissue perfusion and organ hypoxia, thus increasing the risk of mortality. As a result, effective oxygen management has become a critical issue in VA-ECMO therapy.
To date, the direct impact of varying oxygenation targets on patient outcomes during VA-ECMO remains insufficiently validated, with a lack of large-scale randomized controlled trials comparing different oxygenation strategies. Against this backdrop, Aidan et al. proposed two distinct oxygenation strategies: a conservative approach targeting an SaO₂ range of 92-96% and a liberal approach targeting an SaO₂ range of 97-100%. They conducted a multicenter randomized controlled trial to compare the effects of these strategies on both short-term and long-term patient outcomes.
A total of 300 adult patients receiving VA-ECMO treatment were enrolled in the study, including 192 patients with cardiogenic shock and 108 patients with refractory cardiac arrest. All patients were treated in the ICU and randomly assigned to one of two oxygenation target groups based on the inclusion criteria. In the conservative oxygen target group, the ECMO oxygenator and ventilator oxygen concentration were adjusted to maintain the patient's SaO₂ within the range of 92%-96%. In the liberal oxygen target group, the ECMO oxygenator was set to deliver 100% oxygen, while the ventilator oxygen concentration was adjusted to 97%-100%, in order to achieve the target oxygen saturation level.
The results showed no significant difference in ICU-free days between the two oxygenation target strategies (conservative target group: IQR 0-13.7 days; liberal target group: IQR 0-13.3 days), indicating that, in the short term, the oxygen target setting did not significantly impact the speed of patient recovery. Additionally, no significant differences were observed in secondary outcomes, such as mortality, length of hospital stay, and duration of mechanical ventilation, between the two groups. At 6 months, functional assessments revealed no significant differences in disability (WHODAS scores) or quality of life (EQ-5D scores) between the two groups, suggesting comparable functional recovery outcomes. Furthermore, the conservative group (26.8%) exhibited a significantly lower incidence of hyperoxemia compared to the liberal group (43.1%), indicating that the conservative oxygen strategy effectively reduced the risk of excessive oxidative damage. However, during the treatment period, the conservative group experienced more protocol deviations (29.5%), with some patients failing to adhere to the assigned oxygen targets due to clinical reasons.
This study employed a refined intervention method by adjusting both the ECMO oxygenator and ventilator oxygen concentrations to precisely control the patient's oxygen saturation, ensuring the accurate implementation of the oxygen target. This optimization enhanced the stability and consistency of the patient's oxygen supply, preventing issues such as localized hypoxia or hyperoxia that could arise from uneven oxygen distribution. Compared to traditional methods, this approach offers a more precise and personalized oxygen management strategy for clinical use and provides clearer, more scientific evidence for the treatment of VA-ECMO patients.
From a critical perspective, several limitations and gaps remain in this study. First, the use of ICU-free days as a short-term outcome may not fully reflect the effectiveness of the oxygen target strategy. Second, further investigation is needed to explore the stratified effects in different patient populations. Moreover, the study lacks an in-depth evaluation of the patients' long-term quality of life and recovery of organ function. Notably, the high rate of protocol deviations in the conservative oxygen target group underscores the challenges in the clinical implementation of this approach. Future research should optimize the experimental design by focusing on individualized management, multidimensional outcome measures, and potential biological mechanisms, thereby promoting the continued advancement of oxygen target management in VA-ECMO therapy.
REFERENCES:
Burrell A, Bailey M J, Bellomo R, et al. Conservative or liberal oxygen targets in patients on venoarterial extracorporeal membrane oxygenation[J]. Intensive Care Medicine, 2024, 50(9): 1470-1483.






Post comments