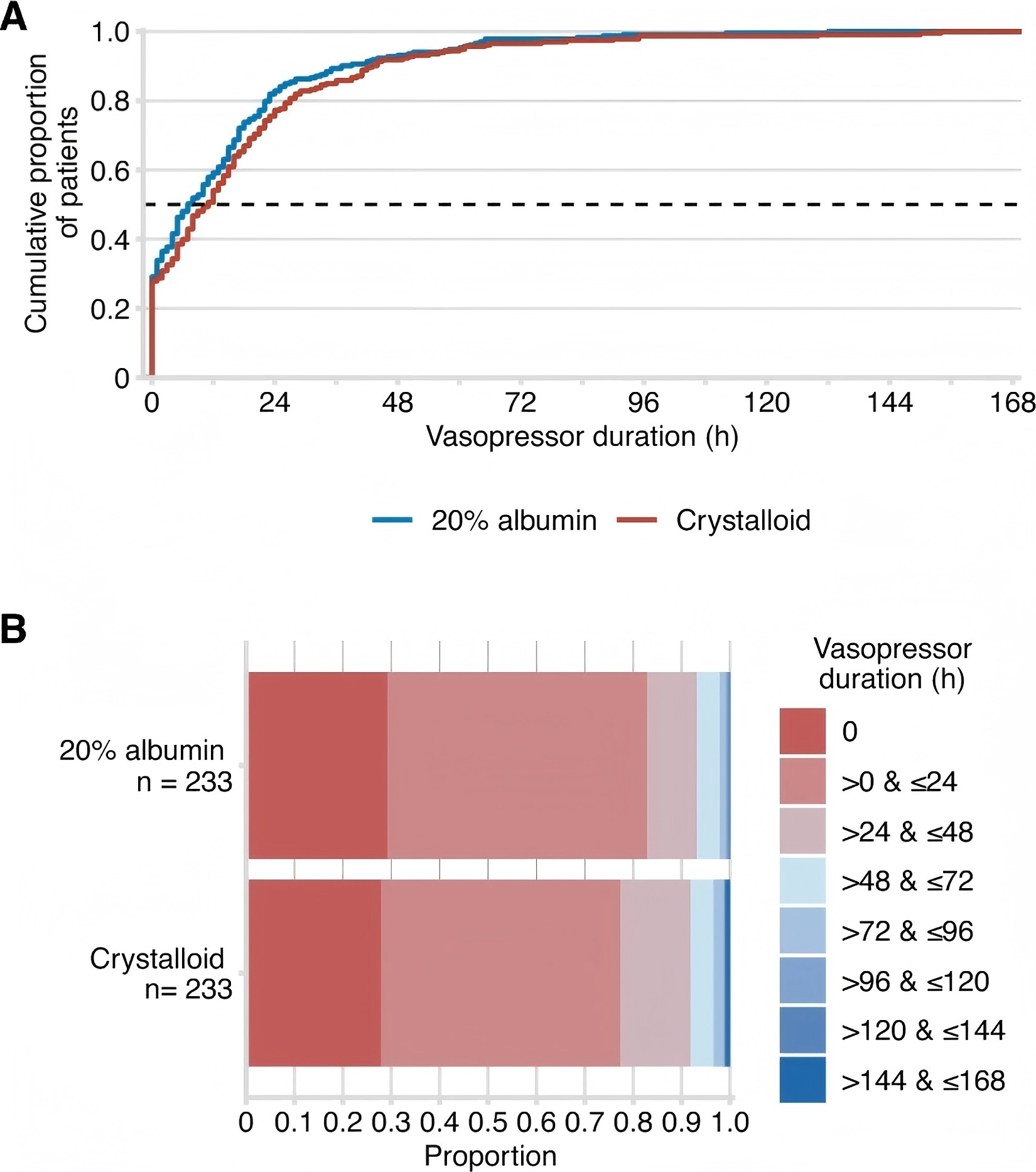
Vasopressor duration. A Distributions of vasopressor hours by study group as the cumulative proportion (y-axis) for each study group by hours (x-axis). Curves that rise faster are more favourable. B Vasopressor hours as horizontally stacked proportions by study group. Red represents better values and blue represents worse values
After cardiac surgery, patients are often at risk of acute hypovolemia and inadequate organ perfusion, making fluid bolus therapy (FBT) a critical method for restoring hemodynamic stability. Among the current fluid treatment options, crystalloids and low-concentration albumin solutions are commonly used, but both carry the risk of fluid overload, which can lead to complications such as edema, pulmonary edema, and ascites. In comparison to these traditional fluids, 20% human serum albumin (HSA) solution, a high-concentration colloid, theoretically offers more effective blood volume expansion at smaller doses due to its high osmotic pressure. This may help reduce fluid-related complications and improve patient outcomes. However, there is insufficient evidence supporting the efficacy of high-concentration albumin in intensive care, particularly in post-cardiac surgery patients. Therefore, the study by Wigmore et al. aimed to evaluate whether 20% HSA solution could effectively reduce the duration of vasopressor use and improve postoperative fluid balance in fluid bolus therapy following cardiac surgery, compared to crystalloids.
This study employed a multicenter, parallel-group, open-label, randomized controlled trial design across six intensive care units (ICUs), enrolling 466 patients who underwent cardiac surgery and required fluid bolus therapy. Patients were randomly assigned to either the 20% HSA group or the crystalloid group. The 20% HSA group received a maximum of 400 mL of 20% HSA daily, with 4% HSA administered if the limit was exceeded, while the crystalloid group initially received 1000 mL of crystalloid solution, with 4% HSA used thereafter if needed.
The study results showed that the median duration of vasopressor use in the 20% HSA group was 7 hours, compared to 10.8 hours in the crystalloid group, with a difference of -3.8 hours (95% CI -8 to 0.4, P = 0.08), which did not reach the predefined level of statistical significance. This suggests that, although 20% HSA may help reduce vasopressor use in the short term, it did not significantly impact the need for hemodynamic support in this study, possibly due to factors such as sample size, patient characteristics, and clinical management strategies.
The study also found that the fluid balance on day 1 in the 20% HSA group was +164 mL, while in the crystalloid group it was +865 mL, with a difference of -701 mL (95% CI -872 to -530, P < 0.001), indicating that 20% HSA significantly reduced postoperative positive fluid balance, thus decreasing the risk of edema. This suggests that 20% HSA may have important clinical significance in reducing fluid overload and preventing edema-related complications.
For secondary endpoints, such as ICU length of stay, mechanical ventilation duration, and mortality rate, no significant differences were observed between the 20% HSA and crystalloid groups. This may indicate that, while fluid therapy has a significant impact on short-term fluid balance, its overall effect on postoperative recovery outcomes requires further validation through additional research.
The innovation of this study lies in its systematic evaluation of the clinical effects of 20% HSA solution in post-cardiac surgery patients through a multicenter, randomized controlled trial. This study addresses a gap in research regarding the application of high-concentration albumin in this patient population. Compared to previous studies, this research not only confirms the benefits of 20% HSA in reducing fluid overload but also provides new insights into fluid therapy, particularly in the selection of fluid types, by proposing a more targeted and potentially advantageous therapeutic strategy.
Although the results suggest that 20% HSA offers advantages in fluid balance and fluid input, the lack of statistical significance in the duration of vasopressor use means that the findings may not be sufficient to support the routine use of 20% HSA as a clinical alternative. Additionally, the open-label design of the study may have introduced observer bias, particularly in the assessment of vasopressor use. Furthermore, the study did not explore the causal relationship between fluid balance changes and long-term outcomes, especially in terms of postoperative complications such as pulmonary edema and infections. Another limitation is the high cost of 20% HSA, which presents a significant barrier to its widespread clinical application. Future research should evaluate its economic efficacy to determine whether it could replace conventional crystalloids or low-concentration albumin.
To better assess the true value of 20% HSA in post-cardiac surgery treatment, future studies should focus on improving blinding techniques, increasing sample size, exploring long-term outcomes, and conducting economic impact analyses.
REFERENCES:Wigmore G J, Deane A M, Presneill J J, et al. Twenty percent human albumin solution fluid bolus administration therapy in patients after cardiac surgery-II: a multicentre randomised controlled trial[J]. Intensive Care Medicine, 2024, 50(7): 1075-1085.






Post comments