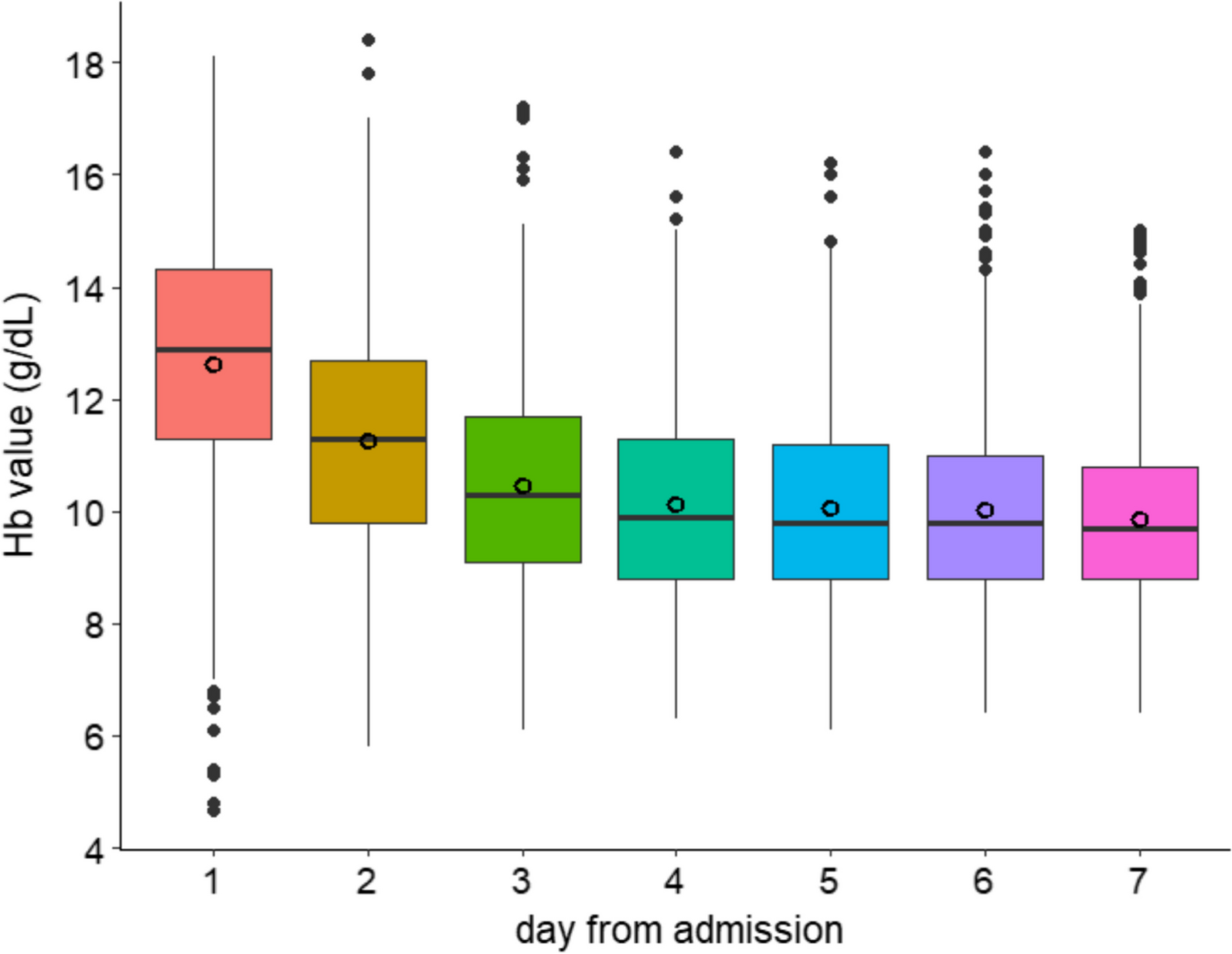
Haemoglobin values during the first week of ICU admission. Distribution of haemoglobin values during the first week of Intensive care unit (ICU) admission. The mean haemoglobin values (empty circles) gradually decreased during the first week from 12.62 (SD 2.2) to 9.8 (SD 1.5) g/dL at day 7
Traumatic brain injury (TBI) is a common and severe condition that frequently necessitates intensive care unit (ICU) treatment. Previous studies have highlighted a strong correlation between the severity of anemia and patient outcomes, making anemia management optimization a crucial focus in medical research aimed at mitigating adverse outcomes. Understanding how fluctuations in hemoglobin (Hb) levels influence the long-term prognosis of TBI patients could help refine clinical treatment strategies. However, the management of Hb levels in TBI patients remains contentious, particularly regarding the optimal Hb thresholds and transfusion strategies, such as restrictive versus liberal approaches, and their effects on long-term outcomes. Against this background, the study by Guglielmi et al. seeks to evaluate the impact of Hb levels on long-term outcomes, including mortality and neurological recovery, in TBI patients, with a focus on different Hb management strategies, in order to offer more precise clinical guidance.
The study utilized data from the CENTER-TBI, a large, multicenter, prospective observational study, and performed a secondary analysis of the lowest Hb values recorded within the first 7 days after admission, aiming to investigate the relationship between these values and neurological outcomes at 6 months. Initially, the researchers classified Hb levels into three groups: <7.5 g/dL, 7.5–9.5 g/dL, and >9.5 g/dL, and employed multivariable logistic regression to control for potential confounding variables. Furthermore, the study examined whether patients had received transfusions, categorizing them into restrictive and liberal transfusion strategies according to clinical guidelines, and further assessed the influence of these transfusion strategies on patient outcomes.
Multivariable regression analysis revealed that higher Hb levels were significantly associated with a reduced incidence of unfavorable neurological outcome. This finding suggests that increasing Hb levels in TBI patients can notably lower the risk of adverse neurological outcomes. Furthermore, the study observed that patients with Hb levels <7.5 g/dL had worse long-term neurological outcomes compared to those with Hb levels >9.5 g/dL, showing a significantly higher risk of unfavorable outcomes. For patients with Hb levels between 7.5 and 9.5 g/dL, although the risk of adverse outcomes was lower, it remained significantly higher than for those with Hb >9.5 g/dL. These results underline the critical importance of early recovery and the maintenance of appropriate Hb levels in improving the long-term outcomes of TBI patients.
In terms of mortality, the study found that higher Hb levels were significantly associated with a reduced risk of death, particularly for patients with Hb <7.5 g/dL, who exhibited a significantly higher risk of death, further emphasizing the detrimental impact of anemia on mortality in TBI patients. This result indicates that timely correction of anemia in TBI treatment not only aids in improving neurological recovery but also significantly reduces mortality.
Regarding transfusion strategies, the study observed that, despite variability in transfusion practices across different centers, both restrictive and liberal transfusion approaches were generally associated with elevated Hb levels, which were strongly correlated with improved patient outcomes. This finding offers a novel perspective for future TBI treatment, emphasizing the critical role of Hb management across various centers and clinical settings to ensure alignment with the goal of optimizing long-term patient outcomes.
Leveraging the large, multi-center CENTER-TBI dataset, this study effectively mitigates the potential sample bias inherent in single-center research, thereby enhancing the generalizability of its findings. Unlike traditional studies that typically focus on the correlation between anemia and TBI prognosis without delving into the specific Hb values and their distinct impacts, this study not only refined Hb classification but also elucidated the differential effects of various Hb levels on neurological outcomes and mortality, thus providing more precise clinical guidance. Additionally, by incorporating an analysis of transfusion strategies, the study revealed the influence of different transfusion thresholds on patient prognosis, offering more tailored treatment guidelines for clinical practice.
However, the study is based on secondary data analysis, which may raise concerns regarding the completeness and quality of the data, particularly considering that treatment variations across different centers could affect the external validity of the conclusions. Additionally, the study relied solely on the Glasgow Outcome Scale-Extended (GOSE) to assess long-term outcomes, neglecting other important factors such as quality of life and mental health. Furthermore, the study did not thoroughly investigate the criteria for transfusion strategies in various clinical scenarios, nor did it explore non-transfusion interventions. Moving forward, in addition to further validating areas of uncertainty, the study will need to address challenges related to data integration, technological implementation, and clinical practice to improve its applicability and robustness.
REFERENCES:Guglielmi A, Graziano F, Bogossian E G, et al. Haemoglobin values, transfusion practices, and long-term outcomes in critically ill patients with traumatic brain injury: a secondary analysis of CENTER-TBI[J]. Critical Care, 2024, 28(1): 199.






Post comments