Acute Brain Injury (ABI) refers to a category of brain dysfunction resulting from trauma, hemorrhage, ischemia, or other factors. It is commonly observed in conditions such as traumatic brain injury (TBI), aneurysmal subarachnoid hemorrhage (aSAH), and intracerebral hemorrhage (ICH). Patients with ABI often require intensive care, and blood transfusion is a common intervention in their clinical management. Maintaining adequate hemoglobin levels is crucial for ensuring sufficient oxygen delivery, particularly because the brain is one of the most oxygen-demanding organs. Low hemoglobin levels may result in inadequate oxygenation of brain tissue, exacerbating brain damage and hindering neurological recovery. Conversely, excessive transfusion can lead to adverse effects, such as infection, immunosuppression, increased blood viscosity, and iron overload, all of which may negatively impact the patient's long-term health.
Although previous studies have investigated various transfusion strategies for trauma and hemorrhagic diseases, there is no consensus on the optimal hemoglobin threshold for ABI, particularly in TBI and hemorrhagic brain injuries. Some studies support a relatively liberal transfusion strategy for TBI and other acute conditions, initiating transfusion when hemoglobin falls below 9 g/dL. This approach is thought to reduce transfusion-related complications, especially in non-hemorrhagic patients. In contrast, other studies advocate a more restrictive transfusion strategy, triggering transfusion only when hemoglobin levels drop below 7 g/dL. This strategy may minimize unnecessary transfusion risks and reduce complications associated with elevated blood viscosity.
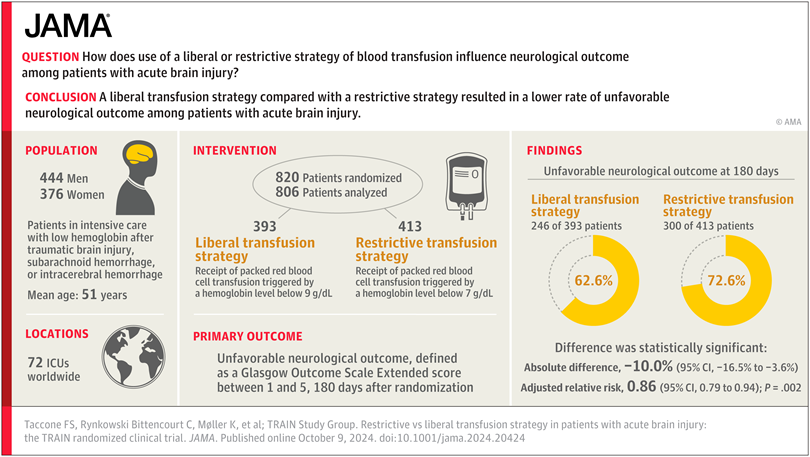
In this context, the study by Taccone et al. investigates the effects of restrictive versus liberal transfusion strategies in ABI patients, with a particular focus on their impact on neurological outcomes. This study is a multicenter, phase 3, parallel-group, investigator-initiated randomized clinical trial conducted across 72 intensive care units (ICUs) in 22 countries. A total of 850 patients with various types of Acute Brain Injury (ABI) were included, with 408 patients assigned to a liberal transfusion strategy and 442 patients to a restrictive transfusion strategy. All patients had hemoglobin levels below 9 g/dL within 10 days post-ABI and were expected to remain in the ICU for at least 72 hours.
The study results indicated that, at the 180-day follow-up, 23.7% of patients in the restrictive transfusion group experienced unfavorable outcomes (GOSE scores 1-5), compared to 25.4% in the liberal transfusion group. The difference between the two groups was not statistically significant (p > 0.05). These findings suggest that, in the management of ABI, there was no significant difference in neurological recovery, regardless of whether a restrictive or liberal transfusion strategy was employed. In other words, the hemoglobin threshold did not significantly influence the neurological recovery of ABI patients.
In addition to the primary outcome, the study also found that the rates of severe adverse events, such as infections and cardiac events, were similar between the restrictive and liberal transfusion groups. Moreover, there was no significant difference in mortality rates between the two groups, suggesting that the restrictive transfusion strategy did not increase the risk of death or adverse events. Regarding transfusion volumes, the liberal transfusion group received a significantly higher average volume of transfusion than the restrictive group, with the liberal group receiving approximately 3.1 units, while the restrictive group received 2.4 units. Despite receiving more transfusion, the liberal group did not demonstrate a clear advantage in neurological outcomes, indicating that increasing hemoglobin levels did not directly contribute to improved neurological recovery.
Compared to previous studies, the strengths of this study lie in its large-scale, multicenter design, which effectively minimizes potential sample bias inherent in single-center studies. More importantly, the study employed a longer follow-up period, providing a more comprehensive assessment of the long-term effects of transfusion strategies on the neurological recovery of ABI patients.
However, despite offering valuable data, the study has several limitations. First, the study did not perform subgroup analyses for different types of ABI, and such analyses could provide more tailored treatment recommendations. Second, the timing of treatment for ABI patients may significantly affect outcomes, particularly whether early transfusion during the acute phase influences brain injury repair. This aspect was not explored in detail in the study. Additionally, further research is needed to investigate transfusion-related immune responses, infection risks, and iron overload.
REFERENCES:Taccone F S, Bittencourt C R, Møller K, et al. Restrictive vs liberal transfusion strategy in patients with acute brain injury: the TRAIN randomized clinical trial[J]. Jama, 2024.







Post comments