In a remarkable leap forward for regenerative medicine, Japanese researchers have successfully conducted the world’s first human trial using induced pluripotent stem cells (iPSCs) to treat corneal diseases. This groundbreaking study, titled “Induced pluripotent stem-cell-derived corneal epithelium for transplant surgery: a single-arm, open-label, first-in-human interventional study in Japan,” marks a significant milestone in the quest to address corneal blindness and vision impairment. Induced pluripotent stem cells, a type of stem cell that can be generated directly from adult cells, have revolutionized the field of regenerative medicine. The discovery of iPSCs was so groundbreaking that it earned Japanese scientist Shinya Yamanaka the Nobel Prize in 2012. These cells have the potential to develop into any type of cell in the body, making them invaluable for regenerative medicine.
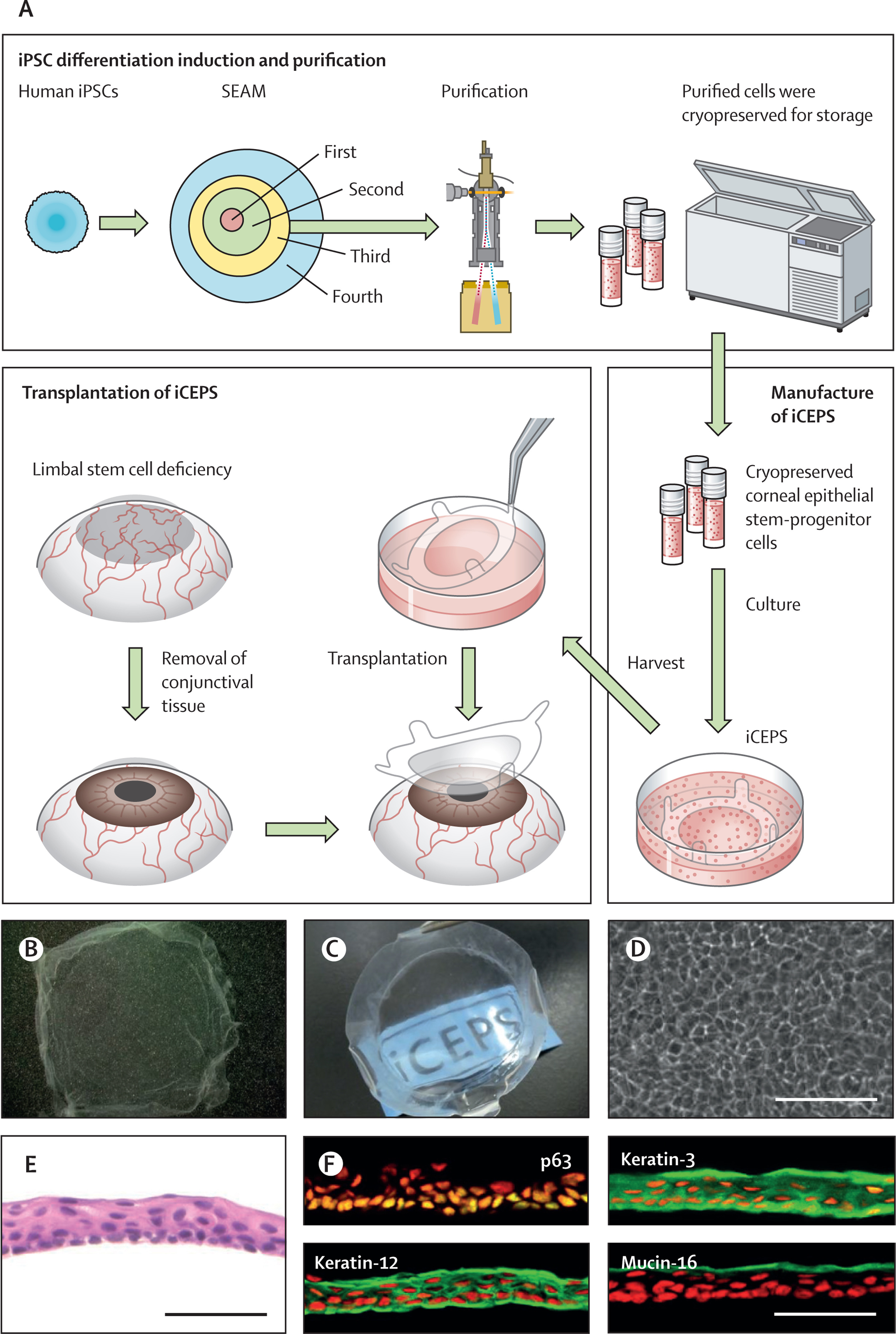
The research team, led by scientists from various Japanese institutions, aimed to evaluate the safety and efficacy of using iPSC-derived corneal epithelial cells for transplantation. The corneal epithelium is the outermost layer of the cornea, which plays a crucial role in maintaining eye health and vision. The study involved patients with corneal epithelial stem cell deficiency, a condition that can lead to vision loss. Researchers created corneal epithelial cells from iPSCs in the laboratory and transplanted them onto the patients’ eyes. The patients were then monitored for one year after the transplantation to assess the outcomes. Encouragingly, the transplanted cells successfully adhered to the corneal surface and showed signs of regenerating the corneal epithelium.This study is of paramount importance because corneal diseases are a leading cause of blindness worldwide, affecting millions of people. Traditional corneal transplants rely on donor tissues, which are often in short supply. This new approach using iPSCs could potentially provide an unlimited source of corneal tissue for transplantation, addressing the global shortage of donor corneas. The use of iPSC-derived corneal cells offers several advantages. Since iPSCs can be created from a patient’s own cells, there’s a lower risk of immune rejection compared to donor transplants. Additionally, lab-grown tissues can be produced under controlled conditions, ensuring consistent quality. This method could potentially produce large quantities of transplantable corneal tissue, meeting the growing global demand.
While the results are promising, the researchers emphasize that this is just the beginning. Long-term follow-up studies are needed to ensure the safety and durability of the transplants. Additionally, larger clinical trials will be necessary before this treatment can become widely available. However, if proven successful in larger trials, this technology could revolutionize the treatment of corneal diseases worldwide. It opens up possibilities not just for corneal transplants, but also for treating other eye conditions and even diseases affecting different organs.
This first-in-human study represents a significant step forward in the field of regenerative medicine. By harnessing the power of iPSCs, researchers are paving the way for innovative treatments that could restore sight to millions of people suffering from corneal diseases. As this technology continues to develop, it holds the promise of transforming lives and offering new hope to those facing vision loss. The success of this trial not only demonstrates the potential of stem cell therapy but also highlights Japan’s position at the forefront of regenerative medicine research. As we look to the future, the possibilities seem both exciting and limitless, with the potential to redefine how we approach treating a wide range of diseases and injuries.
Source:https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(24)01764-1/fulltext






Post comments