By Jonathan Cluett, MD
Medically reviewed by Maria M. LoTempio, MD
Your Achilles tendon helps you walk, jump, and run, so injury to it can be quite debilitating. Treatment for an Achilles tear or Achilles rupture may include a surgical intervention to fix damage to this fibrous connective tissue, helping restore its function and integrity.
If you experience an Achilles rupture, you and your healthcare provider will discuss the risks and benefits of surgical versus non-surgical treatment. Depending on specific characteristics of your tear and relevant factors in your history, your surgeon may recommend surgical treatment of your torn Achilles tendon.1
Ralf Geithe / Getty Images
What Is Achilles Tendon Repair Surgery?
Surgery for Achilles tendon repair involves mending the ends of a torn or ruptured tendon.2 The specific type of surgery will depend on where the Achilles tendon has torn.
If the tendon is torn in the mid substance (above where it attaches to the bone), it will be repaired by reconnecting the two ends with a heavy suture.
If the tendon has torn off of the calcaneus (the heel bone), then the free end of the tendon will be cleaned up, and then it is reattached directly to the bone with special types of bone anchors.
In cases of significant surgical delay or if a significant portion of the tendon has to be removed because it is so unhealthy, your surgeon may have to augment the repair (make it stronger) by rerouting an adjacent tendon in your foot to plug it into the heel bone (tendon grafting), or may have to lengthen the Achilles (make it longer) with special techniques.
Achilles tendon repair is usually done as a scheduled procedure for chronic tears and it is usually done as soon as possible after an acute injury—within a few weeks of it at most.3
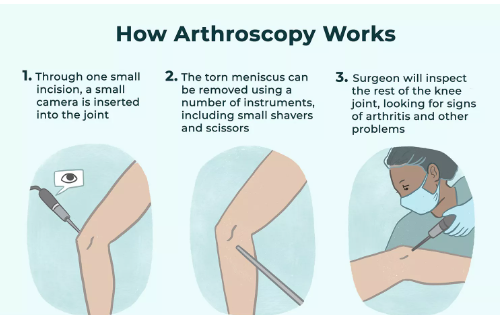
This procedure can be done with an open approach or with a minimally invasive percutaneous approach that relies on several small incisions to repair the tendon with special instruments to bring the ends together. The surgery is performed by an orthopedic surgeon.
Local anesthesia, regional anesthesia (spinal anesthesia), or a nerve block are the usual pain control methods used.4 This means that you will be awake and your pain control will only affect your foot and leg.
Contraindications
Achilles tendon repair surgery isn't the right solution for everyone.
Some relative contraindications include:
Active infection or a wound at the site of the repair, as can occur if there has been a wound complication as the result of an ill applied splint or cast.
A history of blood clots or a new blood clot in the operative leg secondary to the injury. This is very dangerous in the setting of Achilles surgery—which can cause the clot to embolize (move) to the lung.
Being on a blood thinner (for another problem) that can not be stopped during the perioperative period.
Significant pulmonary or cardiac disease may prohibit obtaining medical clearance.
Chronic tendon damage may result in scarring and shortening of the tendon, which can require a different treatment approach.
And if you have a major illness or substantial muscle atrophy (shrinking), you might not be able to participate in postoperative exercises that you need to do to recover—full strength may not be restored even with surgery and therapy.
Surgical repair of a sudden rupture is generally considered more likely to be effective than repair of an older tear because a newly ripped tendon is usually still healthy enough and long enough for the ends to be attached.1
Potential Risks
This surgery can cause complications that are normally associated with anesthesia and surgery.
Infection and healing problems: Achilles tendon repair surgery can be complicated by a post-operative foot infection, impaired wound healing, or impaired healing of the tendon. You would have a higher risk of these issues if you have diabetes or if you're a smoker.
Nerve injury: An injury during the procedure can potentially result in excessive bleeding or nerve damage. An injury to the sural nerve, which closely follows the Achilles tendon along the calf, can lead to numbness or prolonged sensory problems but does not lead to weakness. If a tendon graft is utilized for an acute repair, there is a risk of injury to other major neurovascular structures in the foot.
Blood clot: The risk of a blood clot is higher with Achilles surgery compared with other surgical procedures and often will necessitate treatment. Sometimes a low dose blood thinner is administered immediately following surgery to reduce this risk.
Delayed risks include decreased calf mobility and stiffness due to post-surgical scarring.
There is a risk of a repeat tendon tear after an Achilles tendon repair surgery, even if your surgery is successful.
Purpose of Achilles Tendon Repair Surgery
You might consider having Achilles tendon repair surgery if you have had a total or partial Achilles tendon tear or rupture. This can occur suddenly due to a sports injury or trauma (you might hear a "pop" sound), or it can develop gradually due to repetitive motion.
This type of injury can be diagnosed with a physical examination and non-invasive imaging tests, like a magnetic resonance imaging (MRI) test of your foot. A torn Achilles tendon can cause pain, weakness, and swelling of the foot, so adequate treatment is necessary.
If you have a small tear that is likely to heal without surgery, your healthcare provider might recommend conservative management, such as resting your foot or wearing a cast or brace for several months so the tendon can heal on its own.
However, if the structures of the ripped tendon are not positioned where they could heal properly or the tear is large, it is unlikely to heal on its own.
Because chronic tears might not be easily repaired with surgery, you and your healthcare provider will have to discuss the pros and cons of nonsurgical treatment versus surgery even if you haven't tried conservative management yet.
Sometimes it isn't possible to predict whether conservative management will be effective.
How to Prepare
If you experience a sudden traumatic Achilles tendon rupture, you may have swelling that could interfere with the surgical repair. Your healthcare provider might schedule your repair a few days or a week after your injury to maximize your chances of improvement.
You might have imaging tests for surgical planning, such as an X-ray or MRI of your foot and leg. Additionally, you will have some preoperative testing, including a complete blood count (CBC) and a blood chemistry panel.
Location
An Achilles tendon repair surgery is a scheduled outpatient procedure done in an operating room located in a hospital or surgery center. It is rare to have this procedure immediately after going to the emergency room for an injury.3
What to Wear
You can wear anything comfortable for your surgery appointment. You should wear flat shoes and socks that can easily be removed.
On your way home after surgery, you will have a cast or boot on your surgical foot; you can wear a regular shoe on your other foot.
Food and Drink
You won't have to make any dietary changes for your Achilles tendon repair surgery.
Medications
Your surgeon may adjust some of your regular medications before you have surgery, including blood thinners and anti-inflammatory medications.
What to Bring
When you go to your surgery appointment, it's important that you bring a form of personal identification with you, your health insurance information, and a method of payment for any portion of your surgery that you are required to pay.
Because the surgery is on your foot, you won't be able to drive, so be sure to have someone who can take you home after the procedure.
Pre-Op Lifestyle Changes
Prior to your surgery, you will need to rest your foot to avoid additional injury and help reduce the swelling. This is especially important if you are having surgery for a recent traumatic Achilles tendon rupture.
What to Expect on the Day of Surgery
When you go to your surgery appointment, you will sign in and fill out consent forms. You will then go to a pre-operative area to change into a surgical gown.
Your temperature will be checked, and your pulse, oxygen level, and blood pressure will be monitored. You will have an intravenous (IV, in a vein) line placed before you head to the surgical suite or operating room where you will have your surgery.
Your surgeon will likely see you and examine your foot before your surgery.
Before the Surgery
Your leg will be covered with a drape, and the area where your incision will be placed will be exposed. Your team will clean your foot with a surgical disinfecting cleanser. If you are going to have a tendon transfer, any other area of skin that needs an incision will be cleaned at this time as well.
Depending on the factors specific to your injury and underlying medical conditions, your anesthesia may include light sedation with the use of regional or local anesthesia. Either a regional block to the nerves around the knee or a local block limited to the area of the surgery will provide adequate anesthesia. If you are having a more complex procedure, then other types of regional block, or even a spinal block, may be utilized if it is deemed appropriate or safest by your anesthesiologist.4 General anesthesia is really needed for Achilles tendon repair surgery.
Your healthcare providers will test your sensation to ensure that you can't feel any pain or pressure before your surgery is started.
During the Surgery
Your surgeon will begin your surgery by making an incision along the back of your ankle. Usually, the skin incision is made just to the side of the midline so shoes will not rub on the site of the scar.
Your incision might be several inches long if you are having an open repair, or it can be less than an inch in length if you are having a percutaneous repair. Sometimes a percutaneous repair involves more than one small incision.
You will also have a layer of fascia (connective tissue) cut so your surgeon can access the tendon.
Your surgical team will be able to directly visualize the torn ends of your Achilles tendon if you are having an open procedure.
Strong sutures are placed at both ends of the torn tendon to hold it together. These sutures are then tied together to repair the tissue.
Repair is optimized with the following methods:
Your surgeon will not stretch either end of your torn tendon too much to avoid tears from occurring during or after your surgery.
Generally, the sutures are placed in a strong section of the tendon that won't be ripped by the suture, rather than a frayed or otherwise delicate edge.2
If you need to have a tendon transfer, you will have a section of healthy tendon removed (usually from your foot) and sutured to the torn part of your Achilles tendon to lengthen and/or widen it for repair.
Once your tendon repair is complete, the fascia that was cut will be repaired with sutures, and your surgical device will be removed if you had a percutaneous procedure. Your skin incision will be sutured closed as well.
You will have bandages and surgical dressing placed on your wound. Anesthetic will be discontinued and your anesthesia catheter (if you have one) will be removed.
A cast or brace will be placed on your foot either before you leave the operating room or once you get to the recovery area.
After the Surgery
Your medical team will ask you if you are having any pain after your procedure. You will receive pain medication as needed.
They will also check your foot to make sure you don't have bruising or swelling.
You should receive instructions about wound care, when its OK to place weight on your foot, and when to see your healthcare provider for a follow-up appointment.
Recovery
Your recovery starts with healing, wound care, and a period resting your foot. You will likely need to wear a cast or a removable boot for four weeks. Rehabilitation begins after several weeks of foot immobility and continues for several months.
Your own recovery schedule is based on the size of your incision, the severity of your tendon tear, and your surgeon's overall assessment of your progress in healing.
You will have several appointments with your healthcare provider throughout this phase. Your sutures will be removed and your dressing changed. You will be given direction regarding how and when you can advance your activity and place light pressure on your foot; this usually takes a few weeks.5
Healing
During the healing phase after your surgery, the key goals are to protect your wound and to identify early complications. You will need to make sure that you keep your wound clean and dry as instructed by your medical team, and that you change the dressing based on the instructions you were given.
It's also important that you don't stretch or place pressure on your healing tendon.
Signs of complications include:
Pain
Swelling
Bleeding
Warmth near your surgical site
Fever
Streaks of red on your skin near your cast or dressing
Oozing of fluid or pus
If you develop any of these issues, be sure to call your surgeon's office.
Coping With Recovery
Your foot will be immobilized starting in a pointed position, which helps keep the previously torn ends of the tendon together. Over time, the foot is gradually flexed under the guidance of your healthcare provider.
With this and mobility restrictions, you won't be able to drive for several weeks and you may need to use crutches. To make this time more manageable, ask family and friends with help getting to appointments, grocery shopping, and so on. You may also want to ask for help make modifications to your home, such as moving furniture, to make it easier to get around.
Long-Term Care
You will need to participate in physical therapy and rehabilitation after your surgery. This involves exercises to strengthen the muscles in your calf and foot, as well as to improve your range of motion.
Your surgeon and physical therapist will give you a schedule. Starting therapy too soon can prevent healing, and delaying therapy can lead to muscle atrophy and joint stiffness from lack of use.5
Possible Future Surgeries
You shouldn't need any follow-up surgical procedures after having an Achille's tendon repair operation. However, even with adequately healed repairs, there is a risk of recurrent tearing.
If you have another tear, you and your healthcare provider will consider your likelihood of improving with conservative management or another surgery.
Lifestyle Adjustments
While staying active is highly beneficial for your health, it's important that you are aware of the risks of further injuries. You can try to prevent getting injured by wearing the right shoes for the activities you're doing and aiming for moderate and consistent activity, rather than infrequent high-intensity exercise.
Sources
1.Shi F, Wu S, Cai W, Zhao Y. Multiple comparisons of the efficacy and safety for six treatments in Acute Achilles Tendon Rupture patients: A systematic review and network meta-analysis. Foot Ankle Surg. 2020;S1268-7731(20)30153-3. doi:10.1016/j.fas.2020.07.004
2.Apinun J, Jenvorapoj S, Arirachakaran A, Kongtharvonskul J. Clinical outcomes of chronic Achilles tendon rupture treated with flexor hallucis longus grafting and flexor hallucis longus grafting plus additional augmentation: A meta-analysis [published online ahead of print, 2019 Sep 28]. Foot Ankle Surg. 2019;S1268-7731(19)30154-7. doi:10.1016/j.fas.2019.09.006
3.Park YH, Jeong SM, Choi GW, Kim HJ. How early must an acute Achilles tendon rupture be repaired? Injury. 2017 Mar;48(3):776-780. doi: 10.1016/j.injury.2017.01.020. PMID: 28088376.
4.Lee KT, Park YU, Jegal H, Roh YT, Kim JS, Yoon JS. Femoral and sciatic nerve block for hindfoot and ankle surgery. J Orthop Sci. 2014;19(4):546-551. doi:10.1007/s00776-014-0576-5
5.Baxter JR, Corrigan P, Hullfish TJ, O'Rourke P, Silbernagel KG. Exercise Progression to Incrementally Load the Achilles Tendon [published online ahead of print, 2020 Jul 9]. Med Sci Sports Exerc. July 9, 2020. doi:10.1249/MSS.0000000000002459
By Jonathan Cluett, MD
Dr. Cluett is board-certified in orthopedic surgery. He served as assistant team physician to Chivas USA (Major League Soccer) and the U.S. national soccer teams.






Post comments