By Angelica Bottaro
Medically reviewed by Chris Vincent, MD
Osteoporosis is a disease that causes the bones to become weak and brittle. In people with osteoporosis, bone fractures can occur from something as mild as coughing or bending over. Over time, the fractures caused by osteoporosis can lead to chronic pain, immobility or disability, and even death.1
The bone damage that is done by osteoporosis cannot be reversed. However, you can slow the progression of the disease by building up your bone health and bone density. In some rare cases, people with osteoporosis can revert back to a milder version of bone loss (osteopenia).
DEXA Scans
A dual-energy X-ray absorptiometry, or DEXA, scan is used to help providers determine a person's risk of osteoporosis as well as show how much the disease has progressed. The scan produces a measure of a person's bone density called the T-score.
A diagnosis of osteoporosis versus osteopenia is made based on a measurement that is used to determine how much bone has been lost (T-score).2 If you are on the line between osteoporosis and osteopenia, it might be possible to rebuild your bone density with medication and lifestyle changes. These strategies might help bring your T-score back into the range of osteopenia.
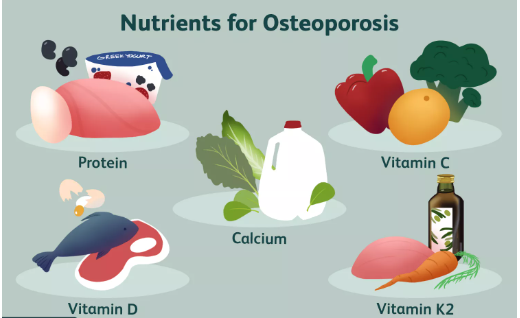
The best way to improve bone loss is to slow the progression of osteoporosis. You can do this by eating a healthy diet that is rich in calcium, vitamins D and K, and protein. Getting regular exercise and taking certain medications that are used to treat osteoporosis (as prescribed by your doctor) might also be recommended.1
How to Prevent Bone Loss
There are several ways that you can prevent bone loss. Lifestyle factors such as diet and exercise as well as the medications you take regularly all influence your levels of bone density and the progression of osteoporosis.
Bisphosphonates
Cells that are designed to degrade bone tissue (osteoclasts) do so throughout a person’s life to allow old bone tissue to be replaced with new bone tissue. The action of osteoclasts is known as resorption. The replacement of old bone tissue with new bone tissue is known as bone remodeling.
In osteoporosis, osteoclasts break down bone tissue that is not replaced, which creates weak and brittle areas.
Bisphosphonates are medications that inhibit the resorption action of osteoclasts, which slows the breakdown of bone tissue.3 Medications of this type, such as Fosamax (alendronate), Actonel (risedronate), and Reclast (zoledronic acid), are the most commonly prescribed to treat osteoporosis.
There are some common and some uncommon side effects that are associated with taking bisphosphonates, including:4
Heartburn or esophagus irritation: The most common side effect can sometimes be prevented by staying upright for 30 to 60 minutes after taking the medication.
Bone cell death of the jawbone and subsequent exposure of the jawbone (osteonecrosis of the jaw): This is a very rare side effect that is usually seen only after dental surgery involving the jaw in people receiving intravenous (IV) doses of bisphosphonates.
Thighbone fractures: This is another rare condition with unclear associations with bisphosphonates use.
Bone, joint, and muscle pain: In some cases, people experience bone, joint, or muscle pain, which may develop right away or years after starting the medication.
Arterial fibrillation: An abnormal heart rhythm may develop in some people; however, research has not yet confirmed it is a true side effect of the medication.
Calcitonin
Calcitonin is a naturally occurring hormone that helps to regulate bone metabolism and calcium levels. It reduces the risk of fractures by increasing bone density, especially in the spine. It is most often given to postmenopausal people with osteoporosis
Some examples of calcitonin medications and how they are given include:
Miacalcin: Nasal spray or injection
Fortical: Nasal spray
Clacimar: Injection
The potential side effects of these medications include nasal irritation, skin flushing, a rash, an increase in urination, and nausea. These side effects are typically mild and do not last long.5
Parathyroid Hormone
Parathyroid hormone (PTH) is another naturally produced hormone that helps to stimulate bone formation. It does so by increasing the number and action of the bone-forming cells (osteoblasts). It also reduces bone breakdown by hindering the cells that break down bones (osteoclasts).6
PTH is typically reserved for people who have been diagnosed with osteoporosis and are at a higher risk of fractures. It can also be used by people who had no results or side effects from other forms of medication.
There are two types of PTH medications:
Forteo (teriparatide), a recombinant version and exact copy of the active portion of the parathyroid hormone protein
Tymlos (abaloparatide), a synthetic version (but not an exact copy) of the same active part of the parathyroid hormone protein. Both are given as a daily injection.
The most common side effects of Forteo (teriparatide) are generalized pain, joint aches, and nausea. Tymlos (abaloparatide) may cause kidney stones (because it increases calcium levels in the urine), dizziness, nausea, headache, irregular heartbeats, fatigue, and upper abdominal pain.7
Hormone Replacement Therapy
People going through menopause experience an accelerated level of bone loss, which can lead to the onset or worsening of osteoporosis. When menopause begins, the levels of estrogen in the body drop significantly. Since estrogen helps protect bones, the reduced levels that occur in menopause mean that protection goes away.8
Estrogen-deficient conditions in younger people (such as hypoestrogenism) can also lead to bone loss.9
Estrogen therapy used to be given frequently to help prevent further bone loss in people who are either deficient in the hormone or are going through menopause. However, because it carries an increased risk of breast cancer, strokes, heart attacks, and blood clots, estrogen is now rarely recommended unless it is prescribed to also control other menopausal symptoms such as hot flashes that are negatively impacting a person's quality of life.9
Selective Estrogen Receptor Modulators
Selective estrogen receptor modulators (SERMs) act in a similar way that estrogen does in the body and have the same effect on bones. They also have anti-estrogen effects on other types of tissues such as breast tissue. SERMs act similarly to hormone replacement therapy (HRT) but do not have the same side effects.
The potential side effects of SERMs can include:10
Leg cramps
Hot flashes
Headaches
Increased sweating
One example of a SERM drug is Evista (raloxifene). It is a pill approved by the Food and Drug Administration (FDA) to be taken by mouth (orally) once per day.
Diet and Supplements
Your diet plays a direct role in bone loss because there are several nutrients that are required to preserve bone density. Specific nutrients your body needs to maintain strong bones include:
Protein: Protein plays a role in how well the body absorbs calcium. Adequate protein intake is vital for bone health.11 Foods rich in protein include eggs, chicken breast, Greek yogurt, almonds, beans, and lean beef. If you do not get enough protein through food sources, you might need to take a protein supplement.12
Vitamin C: Vitamin C may aid in the preservation of bone health by inhibiting osteoclasts from breaking down bone. While the usefulness of vitamin C supplementation in the prevention and treatment of osteoporosis is unproven, experts suggest that it can be helpful to eat a well-balanced diet that includes foods high in vitamin C, such as cruciferous vegetables, bell peppers, potatoes, kiwi, oranges, and tomatoes.13
Calcium: Roughly 99% of the body’s calcium stores are found in the bones and teeth. The mineral is designed to maintain both the structure and the strength of bone. The best way to get calcium is through foods such as dairy products and green leafy vegetables. Many kinds of cereals, breads, and juices are also fortified with calcium. Although calcium is best absorbed through foods, taking a calcium supplement is also an option if you cannot get enough through the foods you eat on a daily basis.14
Calcium and Bisphosphonates
Calcium can affect how well bisphosphonates work. Make sure to talk to your doctor if you are thinking of taking a calcium supplement.14
Vitamin D: Vitamin D is vital for bone health because it helps the body absorb calcium.15 Sun exposure is typically how many people get vitamin D, but it can also be consumed in foods and in supplement form. Some foods that have high levels of vitamin D include oily fish, red meat, egg yolks, and fortified foods.
Vitamin K2: Vitamin K2 may help protect the structural integrity of a specific protein hormone known as osteocalcin. Your body needs this protein because it binds to calcium and helps build and heal your bones. The best source of vitamin K2 is meat, such as chicken, beef, or pork. It can also be found in dark green leafy vegetables, carrots, and vegetable oils. Vitamin K2 supplements have not been proven to prevent osteoporosis fractures.16
Collagen: Collagen is the main protein in bones. It helps to build tissues, ligaments, muscles, and bones. One randomized controlled trial demonstrated that taking collagen supplements for one year was associated with a 4% increase in bone density in the spine and an 8% increase in bone density in the hip. However, it is unknown if taking collagen supplements can prevent osteoporosis-related fractures.17
Medications
Some medications can increase the loss of bone density. In some cases, people with a risk of developing osteoporosis or people who already have the disease will have to avoid medications such as:18
Cortisone (a steroid hormone used to help decrease swelling and inflammation)
Thyroid disease medications
Medications that reduce estrogen levels
Aluminum-containing antacids (such as Maalox, Mylanta, Riopan). (However, antacids containing calcium carbonate, such as Tums and Rolaids, are safe and often recommended as a source of calcium supplementation.)
Other stomach acid–reducing medications (including proton pump inhibitors such as Nexium, Prevacid, and Prilosec)
Selective serotonin receptor uptake inhibitors (SSRIs) (medications used to treat depression and other mental disorders)
Blood thinners
Diuretics (medications designed to rid the body of excess salt)
Anti-seizure medications
When to Talk to Your Doctor
If you are taking medications that might affect your bone density, it's important to talk to your doctor about your options. If you have osteoporosis or are at risk of developing it, you might be able to reduce your dose or take a different medication to help preserve your bone health.
Exercise
Exercise helps with the maintenance and building of bones. During exercise, the muscles and ligaments pull on the bones they are closest to. This action evokes a response in the bone to stimulate more bone cells. Exercise can also help to increase muscle mass, balance, and coordination, which could reduce your risk of falling and getting a fracture.
Research has shown that the best types of exercises to prevent bone loss are resistance training and weight-bearing exercises. Specific exercises that can help with bone loss prevention include:19
Tennis
Dancing
Recreational gymnastics
Squats and lunges
Leg presses
Abdominal exercises such as sit-ups
Lifting weights
Since weight-bearing exercises have been shown to help stimulate bone growth, they are a vital component to reducing bone loss. These types of exercises should be done at least three times a week for a duration of one year for them to have positive effects on bone health.20
Smoking and Alcohol Use
Research has found that tobacco use leads to a decrease in bone density; however, the reason why is complicated. Studies have shown that smoking can also increase the risk of fracture as well as slow bone healing after a fracture has occurred.21
It is thought that smoking could lead to a decrease in bone density through many factors, including:21
Smokers are often thinner and have smaller bones.
Smokers typically exercise less than nonsmokers.
Poor diet is related to tobacco use.
People who smoke tend to go through menopause at an earlier age than nonsmokers.
When it comes to alcohol use, research has found that there is a direct link between heavy drinking and osteoporosis—especially in people who drank heavily during adolescence and early adulthood.
The reason alcohol has such a negative effect on bone health is not well understood; however, people of any age consuming excess amounts of alcohol are found to have lower bone density and greater bone loss.22
Bone Density Screenings
While getting screened regularly for bone density will not help prevent bone loss per se, it will give you the opportunity to stay proactive about your bone health. If you know exactly where you are at in terms of bone loss, you can take the necessary steps to help prevent further bone loss or get the treatment you need to maintain strong and healthy bones.
What to Avoid If You Have Osteoporosis
Smoking and alcohol use can increase your risk of bone loss that could lead to the onset or development of osteoporosis. If you have osteoporosis or are at high risk of developing the disease, avoid smoking cigarettes and limit your alcohol intake.
Summary
Osteoporosis comes with the serious consequences of having weak, brittle bones, such as frequent fractures, which can be debilitating and, in some cases, fatal. That said, whether you already have the disease or are at an increased risk of developing it, there are ways you can help prevent further bone loss and build up your bone density.
Sources
Sözen T, Özışık L, Başaran NÇ. An overview and management of osteoporosis. Eur J Rheumatol. 2017 Mar;4(1):46-56. doi:10.5152/eurjrheum.2016.048
Bone Health and Osteoporosis Foundation. Bone Density Exam/Testing.
Diab DL, Watts NB. Bisphosphonates in the treatment of osteoporosis. Endocrinol Metab Clin North Am. 2012 Sep;41(3):487-506. doi:10.1016/j.ecl.2012.04.007
Health Link BC. Osteoporosis: Should I take Bisphosphonate Medicines.
Pappa HM, Saslowsky TM, Filip-Dhima R, et al. Efficacy and harms of nasal calcitonin in improving bone density in young patients with inflammatory bowel disease: a randomized, placebo-controlled, double-blind trial. Am J Gastroenterol. 2011 Aug;106(8):1527-1543. doi:10.1038/ajg.2011.129
Augustine M, Horwitz MJ. Parathyroid hormone and parathyroid hormone-related protein analogs as therapies for osteoporosis. Curr Osteoporos Rep. 2013 Dec;11(4):400-406. doi:10.1007/s11914-013-0171-2
Haas AV, Leboff MS. Osteoanabolic Agents for Osteoporosis. J Endocr Soc. 2018;2(8):922-932. doi:10.1210/js.2018-00118
National Osteoporosis Foundation. What Woman Need to Know.
Gambacciani M, Levancini M. Hormone replacement therapy and the prevention of postmenopausal osteoporosis. Prz Menopauzalny. 2014 Sep;13(4):213-220. doi:10.5114/pm.2014.44996
U.S. Food and Drug Administration (FDA). Raloxifene Medication Guide.
Mangano KM, Sahni S, Kerstetter JE. Dietary protein is beneficial to bone health under conditions of adequate calcium intake: an update on clinical research. Curr Opin Clin Nutr Metab Care. 2014 Jan;17(1):69-74. doi:10.1097/MCO.0000000000000013
Kerstetter JE, Bihuniak JD, Brindisi J, et al. The Effect of a Whey Protein Supplement on Bone Mass in Older Caucasian Adults. J Clin Endocrinol Metab. 2015 Jun;100(6):2214-2222. doi:10.1210/jc.2014-3792
Brzezińska O, Łukasik Z, Makowska J, et al. Role of Vitamin C in Osteoporosis Development and Treatment-A Literature Review. Nutrients. 2020 Aug 10;12(8):2394. doi:10.3390/nu12082394
Cleveland Clinic. Osteoporosis: Prevention with Calcium Treatment.
Lips P, van Schoor NM. The effect of vitamin D on bone and osteoporosis. Best Pract Res Clin Endocrinol Metab. 2011 Aug;25(4):585-591. doi:10.1016/j.beem.2011.05.002
Capozzi A, Scambia G, Migliaccio S, et al. Role of vitamin K2 in bone metabolism: a point of view and a short reappraisal of the literature. Gynecol Endocrinol. 2020 Apr;36(4):285-288. doi:10.1080/09513590.2019.1689554
König D, Oesser S, Scharla S, et al. Specific Collagen Peptides Improve Bone Mineral Density and Bone Markers in Postmenopausal Women-A Randomized Controlled Study. Nutrients. 2018 Jan 16;10(1):97. doi:10.3390/nu10010097
American Bone Health. Medications That Can Be Bad For Your Bones.
Daly RM, Dalla Via J, Duckham RL, et al. Exercise for the prevention of osteoporosis in postmenopausal women: an evidence-based guide to the optimal prescription. Braz J Phys Ther. 2019 Mar-Apr;23(2):170-180. doi:10.1016/j.bjpt.2018.11.011
Benedetti MG, Furlini G, Zati A, et al. The Effectiveness of Physical Exercise on Bone Density in Osteoporotic Patients. Biomed Res Int. 2018 Dec 23;2018:4840531. doi:10.1155/2018/4840531
National Institutes of Health, Osteoporosis and Related Bone Diseases National Resource Center. Smoking and Bone Health.
National Institute on Alcohol Abuse and Alcoholism. Alcohol and Other Factors Affecting Osteoporosis Risk in Women.
Föger-Samwald U, Dovjak P, Azizi-Semrad U, et al. Osteoporosis: Pathophysiology and therapeutic options. EXCLI J. 2020 Jul 20;19:1017-1037. doi:10.17179/excli2020-2591
Akkawi I, Zmerly H. Osteoporosis: Current Concepts. Joints. 2018 Jun 14;6(2):122-127. doi:10.1055/s-0038-1660790
By Angelica Bottaro
Angelica Bottaro is a professional freelance writer with over 5 years of experience. She has been educated in both psychology and journalism, and her dual education has given her the research and writing skills needed to deliver sound and engaging content in the health space.




Post comments