By James Myhre & Dennis Sifris, MD
Medically reviewed by Anita C. Chandrasekaran, MD
Osteoporosis is thought to be influenced by genetics. This is evidenced by family and twin studies in which 46% to 92% of cases of bone mineral density (BMD) loss are believed to be genetically linked.1
Fractures are the main consequence and concern of osteoporosis. Research suggests that having a first-degree relative with osteoporosis, such as a parent,child, or sibling, increases your risk of an osteoporosis-related fracture by as much as 400%.1
Even so, it is not entirely clear which genes or combination of genes give rise to osteoporosis or how. The available body of evidence suggests that genetics contributes to the incidence of osteoporosis, along with other factors such as older age, a person's sex, and aging-related changes in hormone levels.
Tonpor Kasa / Getty Images
This article takes a closer look at the role that genetics plays in the onset and progression of osteoporosis. It also describes other risk factors associated with osteoporosis and some of the steps you can take to prevent a disease that affects roughly 10 million adults age 50 and over in the United States.2
A Note on Gender and Sex Terminology
Verywell Health acknowledges that sex and gender are related concepts, but they are not the same.
Sex refers to biology: chromosomal makeup, hormones, and anatomy. People are most often assigned male or female at birth based on their external anatomy; some people do not fit into that sex binary and are intersex.
Gender describes a person's internal sense of self as a woman, man, nonbinary person, or another gender, and the associated social and cultural ideas about roles, behaviors, expressions, and characteristics.
Research studies sometimes don't use the terminology in this way. For example, terms that describe gender (“woman,” “man”) may be used when terms for sex (“female,” “male”) are more appropriate.
To reflect our sources accurately, this article uses terms like "female," "male," "woman," and "man" as the sources use them.
How Osteoporosis Develops
Osteoporosis is the most common cause of bone fractures in adults over 70.2 The disease is caused by an imbalance between bone resorption (the breakdown of bone minerals) and the formation of new bone in a process known as bone remodeling.3
Bone remodeling ensures that bone strength is maintained by constantly breaking down and rebuilding older bones a little at a time. Vitamin D and calcium play a central role by triggering bone resorption and formation, respectively. Vitamin D also aids in the absorption of calcium.4
If any part of the remodeling process is imbalanced, bones can start to thin, become brittle, and break.
One cause for the disruption of the process is aging-related changes in hormone levels. This includes natural declines in the sex hormone estrogen after menopause in people who menstruate, which leads to more bone resorption than formation.4
On the flip side, natural increases in parathyroid hormone (PTH) in both people of any sex cause calcium to leave the bones and go into the blood, leading to bone mineral loss.4
It is for these and other reasons that osteoporosis tends to affect people over 50, most especially postmenopausal females.2
Genetics is known to further predispose a person to osteoporosis, while various lifestyle factors (including nutritional deficiencies, physical inactivity, cigarette smoking, and alcohol use disorder) can amplify the risk.3
The Role of Genetics in Osteoporosis
While older age and a low BMD are strong predictors of osteoporosis-related fractures, a family history of osteoporosis also greatly influences the risk. Studies have shown that having a sibling with a low BMD increases your risk of a low BMD by sixfold compared to the general population.5
Yet, despite the strong statistical evidence for the heritability of osteoporosis, there remain large gaps in scientists' understanding of how genetics factors into the development and risk of osteoporosis.
The Search for the "Osteoporosis Gene"
To better understand how genetics influences bone mineral loss, researchers in the early 2000s turned to the human genome—the complete map of genetic (DNA) instructions in humans—to search for gene variations common in people with osteoporosis.
Much of the early research was focused on twins in whom certain genes were abnormally positioned on the chromosomes of both people.1
Based on these and other studies, scientists have identified genetic variants linked to osteoporosis and variants linked to osteoporosis in specific parts of the body (such as the hip or lower spine).5 Other variants still are able to predict a person's risk of a fracture from osteoporosis based on the pattern of bone mineral loss.6
Osteoporosis Gene Variants
To date, no fewer than 71 genetic variants associated with osteoporosis have been found.1 Some of the associations are stronger than others, and it is possible that multiple genetic variants may contribute to the overall risk of the disease.7
Possible Mechanisms
Despite progress in genetic research, scientists have yet to establish a clear association between osteoporosis and the different genetic variants.
While certain variants may predispose you to osteoporosis, having one or even several variants doesn't mean you will get osteoporosis. Other factors, such as a person's age, weight, and sex, can ultimately determine how consequential (or inconsequential) a variant is.1
Scientists today believe that the different genetic variants contribute to osteoporosis by interfering with specific, unique processes involved in bone remodeling.
These include:5
Wnt signaling pathway: This is a process in which secreted proteins enable communication between cells in order to repair bones and regulate and maintain bone mass Variants that can interfere with this process include AXIN1, CTNNB1, DKK1, GPR177, JAG1, LRP4, LRP5, MEF2C, RSPO3, SFRP4, SNT16, SOST, WNT4, WNT5B, and WNT16.
RANK-RANKL-OBG pathway: This is a process in which secreted proteins activate and differentiate the various types of bone cells (called osteoclasts) that make up bones. Variants that can interfere with this include mutations of the TNFRSF11, TNFRSF11A, and TNFRSF11B genes.
Endochondral ossification: This is a process in which the cartilage scaffolding within bones is replaced by bone minerals during remodeling. Variants that can interfere with this include IBSP, PTHLH, RUNX2, SOX6, SOX9, SPP1, and SP7.
By better understanding how genes contribute to the onset or progression of osteoporosis, scientists may one day be able to develop drugs that can block these and other processes that contribute to bone mineral loss.
Other Risk Factors
Even beyond a person's age and genetic predisposition for osteoporosis, there are numerous other factors that can contribute to the overall risk of bone mineral loss. Some factors are modifiable (changeable), while others are unmodifiable (unchangeable).
The most common risk factors for osteoporosis include:
Female Sex
Females 50 and over have a fourfold greater risk of osteoporosis compared to their male counterparts. This is not only due to declines in estrogen during menopause but also because females tend to have smaller frames and have less bone mass to draw upon as they age.8
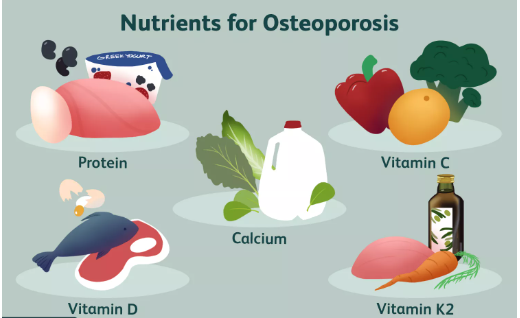
Nutritional Deficiencies
Malnutrition plays a major role in osteoporosis by depriving the body of the nutrients needed to maintain bone health, most notably calcium and vitamin D.9 In the United States, malnutrition is common, affecting no less than 50% of older adults, according to the Department of Health and Human Services.10
But calcium and vitamin D are only part of the picture. The inadequate intake of protein contributes to osteoporosis-related fractures by reducing BMD and the muscle strength needed to support weakened bones.9
Cigarette Smoking
Studies suggest that osteoporosis is more common among smokers than non-smokers (75% versus 52.7%, respectively). Researchers have found that cigarette smoke causes bone mineral loss both directly and indirectly:11
Smoking directly affects BMD by reducing blood circulation needed for bone resorption and formation. This, in turn, leads to imperfect bone formation.
Smoking indirectly affects BMD by impairing the absorption of calcium. It also alters estrogen and PTH levels.
Alcohol Use Disorder
Chronic, heavy alcohol use decreases bone density and destabilizes the matrix of osteoclasts that give bones their strength and resistance to impact.12 It does so by interfering with the production of vitamin D, which calcium needs to be absorbed. Without ample calcium, bone formation is weakened.13
Alcohol and Hormone Levels
Chronic, heavy alcohol use can also reduce estrogen levels in females and testosterone levels in males, both of which contribute to bone mineral loss and impaired bone remodeling.13
Medical Conditions
Any chronic medical condition that interferes with the process of bone remodeling can contribute to osteoporosis. It can do so by causing nutritional deficiencies, impeding the absorption of calcium or vitamin D, altering hormone levels, or provoking a chronic inflammatory response that disrupts the normal production of osteoclasts.14
These include medical conditions such as:14
Anorexia nervosa
Cancer
Celiac disease
Chronic kidney disease (CKD)
Diabetes
Gastric bypass surgery
Inflammatory bowel disease (IBD, including Crohn's disease and ulcerative colitis)
Liver disease
Lupus
Multiple sclerosis (MS)
Rheumatoid arthritis
Thyroid disease
Medications
Many drugs can affect bone metabolism. Some affect hormone levels, inhibit calcium absorption, disrupt the balance of vitamin D and calcium, or interfere with bone resorption.14
Substances affecting the bones include:14
Antidepressants, including selective serotonin reuptake inhibitors (SSRIs)
Chemotherapy drugs, especially aromatase Inhibitors
Corticosteroids (steroids) like prednisone
Depo-Provera (medroxyprogesterone acetate; an injectable contraceptive)
Immunosuppressants like cyclosporine or calcineurin Inhibitors
Proton pump inhibitors (PPIs)
Thiazolidinediones
Thyroid hormones like Synthroid (levothyroxine)
Coumadin (warfarin)
Race/Ethnicity
Data from the ongoing National Health and Nutrition Examination Survey (NHANES) has shown that osteoporosis generally is diagnosed more often in White people (50.8%) compared to Latinx people (44%) or Black people (23.7%).15
It is unclear what role genetics may play in this, but researchers have identified several factors that may contribute to the disparity:15
Among White people, a family history of osteoporosis, vitamin D deficiency, or the daily use of corticosteroids is associated with greater BMD loss.
Among Black people, type 2 diabetes (a disease that is four times more common in Blacks than Whites) is linked to an increased risk of low BMD.
Among all racial/ethnic groups, older age, female sex, and a history of fractures are linked to a higher risk of osteoporosis.
Getting Screened for Osteoporosis
Osteoporosis is diagnosed when a person's BMD falls below 2.5 standard deviations (SDs) of the BMD of the average healthy, young adult. (A standard deviation is a statistical value used to describe the amount of variation from the norm.)16
Osteoporosis is currently defined as follows:16
Normal bone mass: BMD is within 1 SD of the BMD of the average healthy young adult.
Low bone mass: BMD is 1 and 2.5 SD below the BMD of the average healthy young adult.
Osteoporosis: BMD is 2.5 SD or more below the BMD of the average healthy young adult.
Severe osteoporosis: BMD is 2.5 SD or more below the BMD of the average healthy young adult., plus the person has at least one osteoporosis-related fracture.
BMD is typically measured with an imaging tool called a dual-energy X-ray absorptiometry (DEXA) scan. A DEXA scan works by using two different X-ray beams to differentiate bone from other tissues. It is a simple, noninvasive imaging tool that delivers a low radiation dose and does not involve drugs or contrast agents.
Who Should Be Screened?
The U.S. Preventive Services Task Force (USPTF) recommends osteoporosis screening for all females 65 years of age and older as well as postmenopausal females under 65 with risk factors for osteoporosis.17
The USPTF has not offered any recommendations regarding osteoporosis screening in males due to the lack of evidence supporting its benefits.17
Prevention Tips for Those at Increased Risk
While some risk factors for osteoporosis are unmodifiable, there are others you can change, despite your genetic predisposition for the disease.
According to the National Institute on Aging, the five key measures you can take to prevent osteoporosis or the risk of fractures from osteoporosis are:18
Eat foods that support bone health: This includes ensuring you meet the recommended daily intake of calcium, vitamin D, and protein. Good sources include low-fat dairy, grains, fish, and leafy green vegetables.
Take a supplement: If your vitamin D levels are low, speak with your healthcare provider about taking a vitamin D supplement.
Exercise routinely: Weight-bearing exercises can help build and strengthen your bones. Examples include strength training, walking, jogging, hiking, tennis, and dancing.
Limits your alcohol intake: Dietary guidelines recommend no more than two alcoholic beverages per day for males and one alcoholic beverage per day for females. If you have trouble with your drinking, speak with your healthcare provider about alcohol treatment.
Quit cigarettes: Ask your healthcare provider about smoking cessation aids, many of which are fully covered under the Affordable Care Act.
Summary
Genetics is thought to predispose certain people to osteoporosis, particularly those with a family history of the disease. Even so, there remain questions as to how genes influence the risk of osteoporosis and which genes (or combination of genes) are most likely to cause bone mineral loss.
In the end, genes only play a part in a person's overall risk of osteoporosis in tandem with other risk factors such as older age, smoking, alcohol abuse, malnutrition, and co-occurring medical conditions.
There are numerous things you can do to prevent or slow the progression of osteoporosis. Many of these "fixes" are the same healthy choices you would make if you were trying to prevent heart disease, diabetes, or other common chronic diseases. If you need help, speak with your healthcare provider, who can also refer you to a nutritionist, personal trainer, or other health professionals.
Sources
Mullin BH, Walsh JP, Zheng HF, et al. Genome-wide association study using family-based cohorts identifies the WLS and CCDC170/ESR1 loci as associated with bone mineral density. BMC Genomics. 2016;17:136. doi:10.1186/s12864-016-2481-0
Clynes MA, Harvey NC, Curtis EM, Fuggle NR, Dennison EM, Cooper C. The epidemiology of osteoporosis. Br Med Bull. 2020;133(1):105–117. doi:10.1093/bmb/ldaa005
Liang B, Burley G, Lin S, et al. Osteoporosis pathogenesis and treatment: existing and emerging avenues. Cell Mol Biol Lett. 2022;27:72. doi:10.1186/s11658-022-00371-3
Bhattarai HK, Shrestha S, Rokka k, Shakya R. Vitamin D, calcium, parathyroid hormone, and sex steroids in bone health and effects of aging. J Osteoporos. 2020;2020:9324505. doi:10.1155/2020/9324505
Clark GR, Duncan EL. The genetics of osteoporosis. Br Med Bull. 2015;113(1):73-81. doi:10.1093/bmb/ldu042
Nielson CM, Liu CT, Smith AV, et al. Novel genetic variants associated with increased vertebral volumetric BMD, reduced vertebral fracture risk, and increased expression of SLC1A3 and EPHB2. J Bone Miner Res. 2016;31(12):2085–2097. doi:10.1002/jbmr.2913
Makitie RE, Contantiti A, Kampe A, et al. New insights Into monogenic causes of osteoporosis. Front Endocrinol (Lausanne). 2019;10:70. doi:10.3389/fendo.2019.00070
Alswat KA. Gender disparities in osteoporosis. J Clin Med Res. 2017;9(5):382–387. doi:10.14740/jocmr2970w
Munoz-Garach A, Garcia-Fontana B, Munoz-Torres M. Nutrients and dietary patterns related to osteoporosis. Nutrients. 2020;12(7):1986. doi:10.3390/nu12071986
Administration of Community Living. Combatting senior malnutrition.
Al-Bashaireh AM, Haddad LG, Weaver M, Chenggou X, Kelly DL, Yoon S. The effect of tobacco smoking on bone mass: an overview of pathophysiologic mechanisms. J Osteoporos. 2018;2018:1206235. doi:10.1155/2018/1206235
National Institute on Alcohol Abuse and Alcoholism. Alcohol and other factors affecting osteoporosis risk in women.
National Institutes of Health. What people recovering from alcoholism need to know about osteoporosis.
Mirza F, Canalis E. Secondary osteoporosis, pathophysiology and management. Eur J Endocrinol. 2015;173(3):R131–151. doi:10.1530/EJE-15-0118
Zheng XY, Zhou A, Gao Y, et al. Racial differences and factors associated with low femoral neck bone mineral density: an analysis of NHANES 2005–2014 data. Arch Osteoporos. 2021;16:9. doi:10.1007/s11657-020-00850-0
National Institute of Arthritis and Musculoskeletal and Skin Diseases. Bone mass measurement: what the numbers mean.
U.S. Preventive Services Task Force. Osteoporosis to prevent fractures: screening.
National Institute on Aging. Osteoporosis.
Lee J, Lee S, Jang S, Ryu OH. Age-related changes in the prevalence of osteoporosis according to gender and skeletal site: th Korea National Health and Nutrition Examination Survey 2008-2010. Endocrinol Metab (Seoul). 2013;28(3):180–191. doi:10.3803/EnM.2013.28.3.180
Gallagher JC, Tella SR. Prevention and treatment of postmenopausal osteoporosis. J Steroid Biochem Mol Biol. 2014;142:155–170. doi:10.1016/j.jsbmb.2013.09.008
By James Myhre & Dennis Sifris, MD
Dr. Sifris is an HIV specialist and Medical Director of LifeSense Disease Management. Myhre is a journalist and HIV educator.






Post comments