—Edited from <Yale-G First Aid: Crush USMLE Step 2CK and Step 3> By Yale Gong, M.D., Sr. Medical Advisor at www.medicine.net (Copyrighted)
Credit:www.freepik.com
Blood pressure generally refers to systemic arterial blood pressure, the force driving blood flow through arteries, and the lateral pressure exerted by blood on arterial walls. Arterial blood pressure (ABP) is determined by four factors: ventricular contraction, circulating blood volume, arterial wall compliance, and peripheral arterial resistance. Hypertension (high blood pressure, HBP) is defined as a persistent elevation in systemic arterial blood pressure. It is a common clinical syndrome that can lead to serious pathologic changes in the heart, brain, kidneys, blood vessels, and eyes.
1. How can hypertension be diagnosed?
Normal blood pressure for adults is below 120/80 mmHg. However, changes in an individual's health may alter their blood pressure. Clinically, hypertension is defined as blood pressure measured on three separate occasions exceeding 130/80 mmHg. If blood pressure exceeds 180/110 mmHg with evidence of cardiovascular disease (CVD), a diagnosis of hypertension can be confirmed after a single visit.
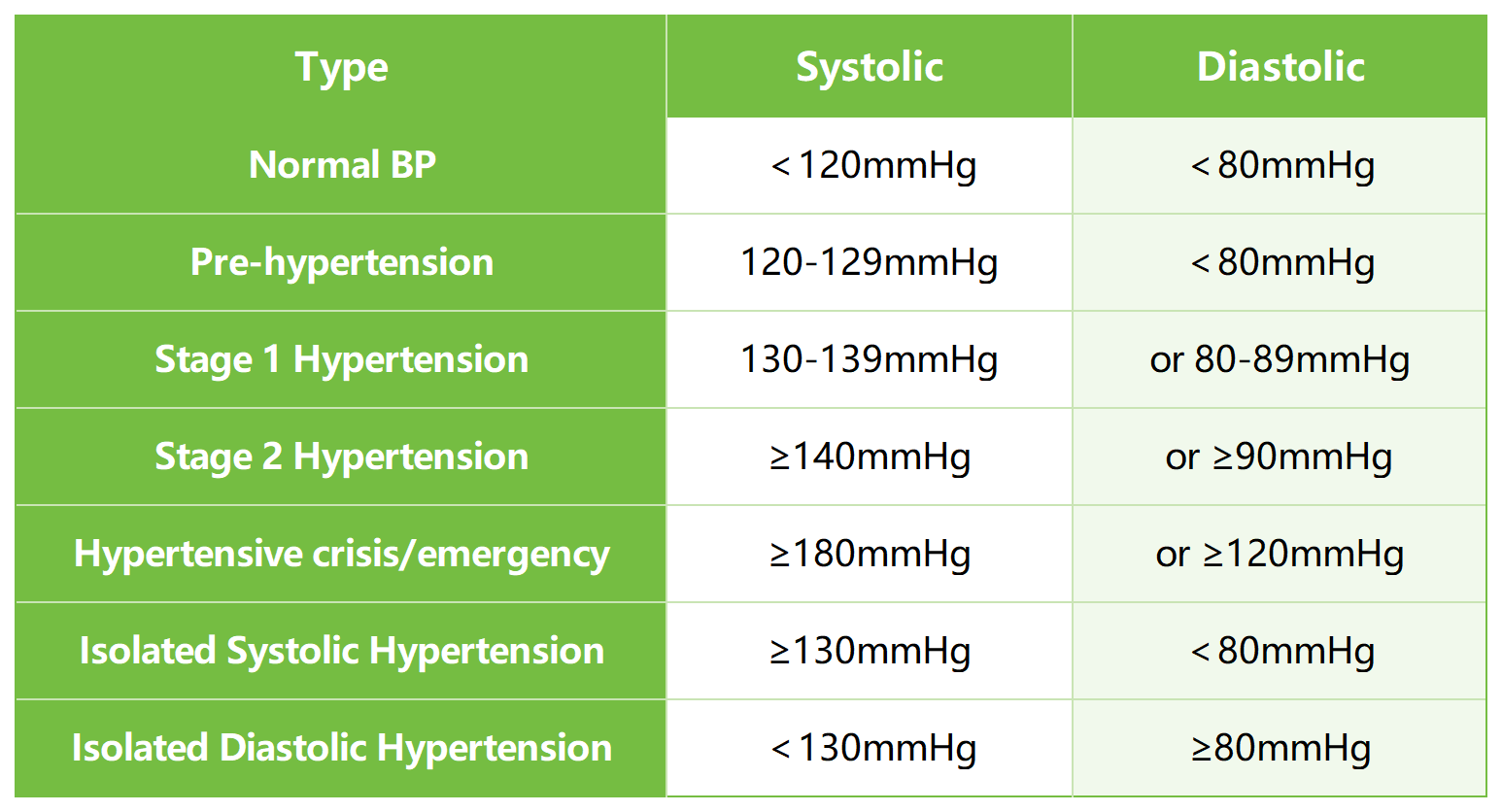
2. What are the categories and stages of hypertension?
Hypertension by causes can also be categorized as primary and secondary hypertension. Primary (essential) hypertension has no clear known causes and accounts for 95% of clinical cases. Secondary hypertension follows clear causes as below.
Hypertension in adults is divided into several stages, each carrying significant health risks. One classification is based on systolic and diastolic pressure, divided into pre-hypertension, stage 1 hypertension, stage 2 hypertension, Hypertensive crisis/emergency, isolated systolic hypertension, and isolated diastolic hypertension.
3. What are the causes, risk factors and associated diseases of hypertension?
Primary hypertension has no known causes but carries risk factors such as family history of hypertension or heart disease, prolonged neuroendocrine stress, high-salt diets, smoking, obesity, advanced age, and reduced physical activity.
Secondary hypertension is caused by specific organic conditions, such as long-term substance use (including alcohol, estrogen, NSAIDs, cocaine, etc.), renal diseases (glomerulonephritis, renal artery stenosis, polycystic disease), endocrine disease (primary aldosteronism, Cushing syndrome, tumors), or pregnancy after 20 weeks of gestation.
4. How to choose the best therapies and medications according to an individual’s conditions?
Adopting a healthy lifestyle is the primary strategy for preventing and treating primary hypertension and reducing risks of its complications. Lifestyle modifications include regular exercise, weight management, limiting alcohol consumption, and following a BP-lowering diet—with reduced salt, fat, sugar, and red meat, and increased vegetables, fruits, whole grains, fish, and nuts.
If lifestyle changes alone cannot effectively control hypertension, medication becomes essential. For isolated hypertension, initial treatment typically involves a single medicine, primarily from these four types:
(1)Thiazide diuretics: such as chlorthalidone, indapamide.
(2)Long-acting calcium channel blockers (CCBs): such as amlodipine.
(3)Angiotensin-converting enzyme inhibitors (ACE-Is).
(4)Angiotensin II receptor blockers (ARBs).
For ischemic stroke cases in acute phases, antihypertensive drugs are generally not administered unless BP is ≥185/110 mmHg.
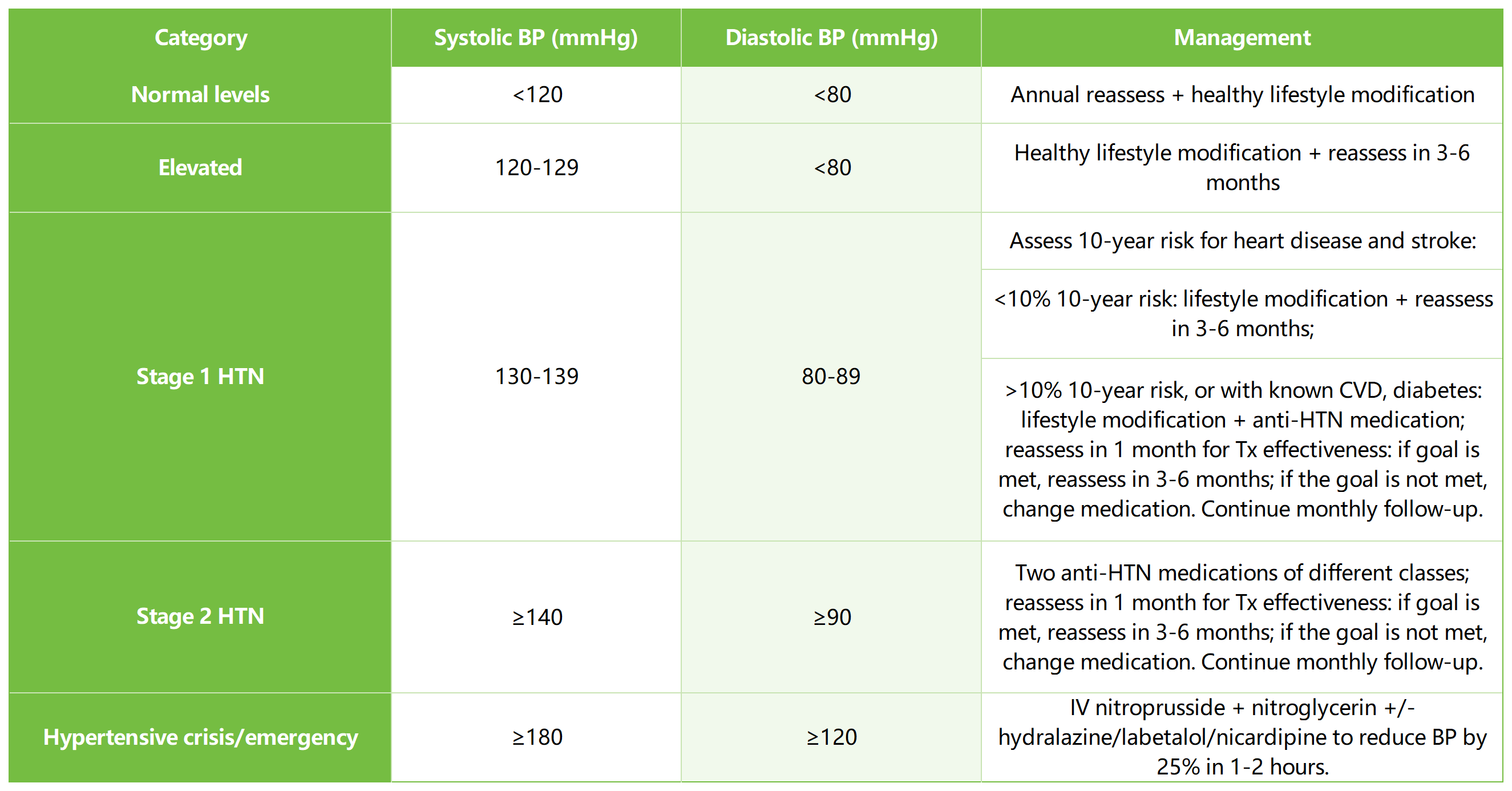
Summary: Blood Pressure Staging and Management
(Edited from American College of Cardiology and American Heart Association)
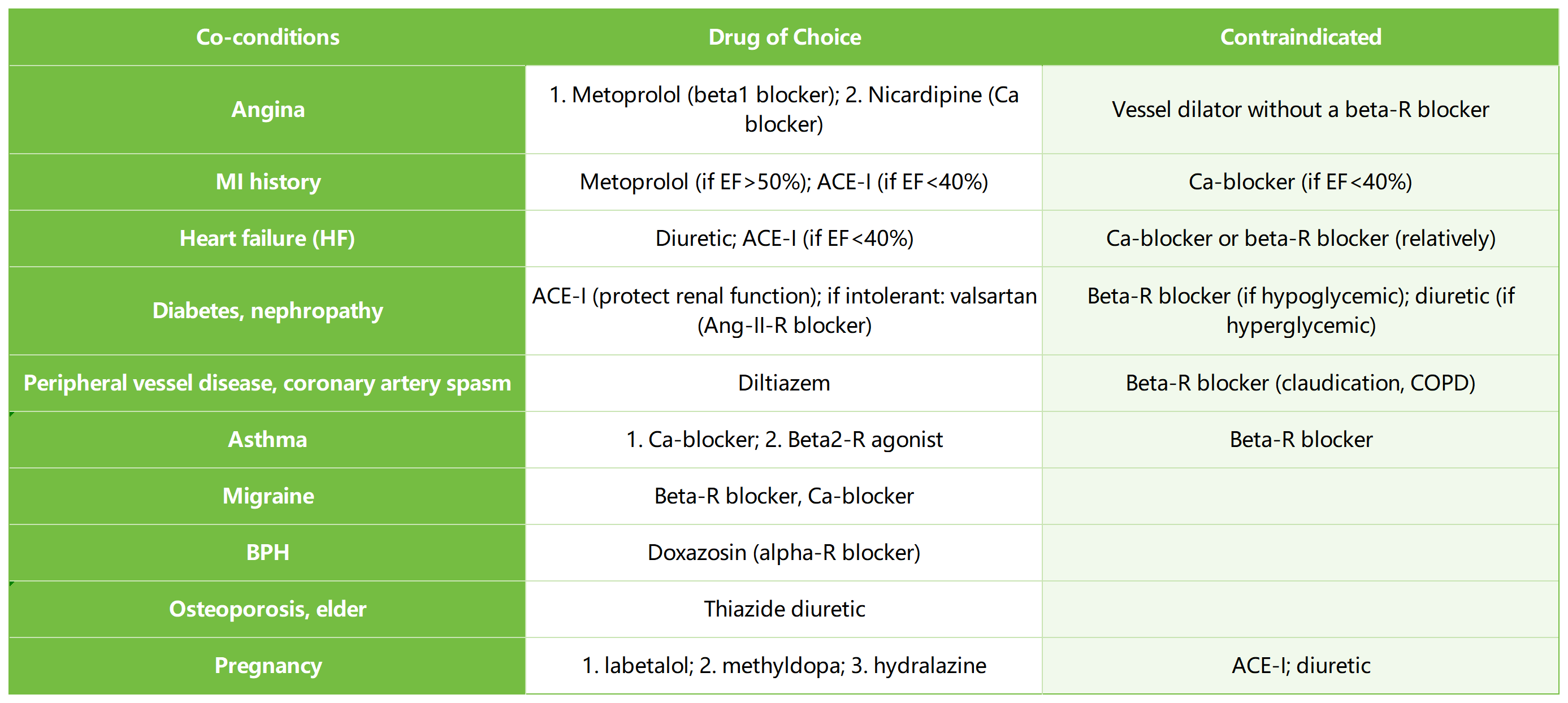
The best selection of antihypertensives is based on specific conditions of the patient, as summarized in the table below (“precision medicine”).
For secondary hypertension, which is caused by a specific condition, cause-treatment is necessary, such as cessation of responsible substances, proper medications, or targeted surgery to a renal disease.







Post comments