A biopsy is often not needed
By Colleen Doherty, MD
Medically reviewed by Robert Burakoff, MD
Liver cancer (also called hepatocellular carcinoma) occurs when abnormal cells in the liver begin to grow uncontrollably. Generally speaking, the diagnosis of liver cancer involves the following steps—a physical examination, blood tests, imaging and sometimes a biopsy.1
Depending on whether or not you have been previously diagnosed with chronic liver disease and/or cirrhosis, which is when the liver irreversibly scars as a result of chronic liver disease, your healthcare provider may proceed a bit differently with diagnosing liver cancer.
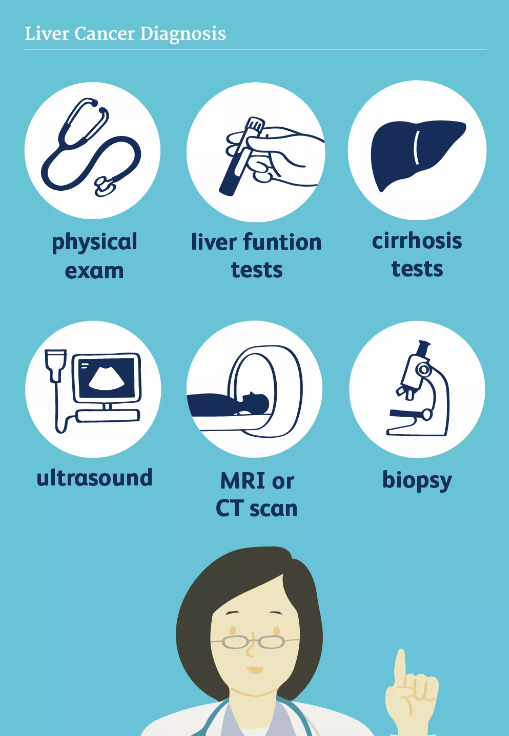
Physical Examination
After reviewing your risk factors for liver cancer (for example, whether you have a history of cirrhosis or a history of alcohol abuse), if your healthcare provider is suspicious for cancer, he will pay close attention to your abdomen, especially the right side where your liver is located. More specifically, your practitioner will press beneath your right ribcage in order to determine if your liver is enlarged.
Your healthcare provider will also look for other signs of long-term liver disease (which increase your risk of having liver cancer) like:2
An enlarged spleen, located in the upper left side of your abdomen
Visible veins on your abdomen
A fluid-filled, swollen abdomen
Evidence of jaundice (for example, yellowing of the white part of your eye
Labs
There are a number of blood tests your healthcare provider may order to help diagnose liver cancer and determine the potential cause of the cancer.
Alpha-Fetoprotein (AFP) Tumor Marker
AFP is a protein that is high in fetuses but falls to low levels after birth.
Interpreting your AFP blood test result can be tricky. For one, a person can have liver cancer and their AFP level may still be normal (it simply hasn’t risen yet). Moreover, high AFP levels may be elevated for other reasons besides liver cancer (for example, cirrhosis or chronic active hepatitis).
The bottom line is that while a helpful test, an AFP level is not a definitive blood test for diagnosing liver cancer—it’s simply one piece of the puzzle.1
Cirrhosis Tests
If a physical exam or imaging test reveals that you have chronic liver disease and/or cirrhosis, but the cause behind it has not yet been determined, your healthcare provider will order a series of blood tests. For instance, he will order blood tests to check for infection with hepatitis B and C. He will also likely order ferritin and iron levels to check for hemochromatosis, another common cause of cirrhosis.3
Liver Function Tests (LFTs)
LFTs comprise a series of blood tests that give your practitioners an idea of how well your liver is functioning.4 These tests can also help your healthcare provider figure out the best treatment plan for your liver cancer. For instance, if your liver cancer is small and contained and your liver appears to be working well, then removing the cancer by surgery may be a sensible option.
Other Tests
Your practitioner may order other blood tests to determine how well other organs in your body are working. For example, he may order blood tests that evaluate how well your kidneys are working. Additionally, since liver cancer may impact blood levels of glucose, calcium, and platelets, these tests may also be ordered.
Imaging
Imaging tests are essential to diagnosing liver cancer.5
Ultrasound
The first test a person may undergo is an ultrasound. During an ultrasound, a probe will be gently pressed on your abdomen to see if there are any masses located in your liver.
CT Scans and MRIs
If a mass is seen on an ultrasound, a more sophisticated test like a computed tomography (CT scan) and/or magnetic resonance imaging (MRI) of the liver is done to give more detailed information about the mass, such as:
Size
Location in the liver
Spread to nearby blood vessels or other parts of the abdomen
These imaging tests may also give information about what type of mass is present, meaning whether the mass is benign (noncancerous) or malignant (cancerous).
Angiography
Lastly, a CT angiography or MRI angiography may be performed to provide a picture of the arteries supplying blood to the liver. For this test, you will need an IV placed in your arm so that contrast dye can be administered during the CT scan or MRI.
Biopsy
During a liver biopsy, a needle is placed through the skin of your abdomen into the liver mass. To minimize any discomfort, the area of skin where the needle is going is numbed beforehand. Cells from the mass are removed and then examined by a healthcare provider (called a pathologist) to see if cancer is present.
Sometimes a biopsy of the liver mass is done during surgery (called a surgical biopsy). With this type of biopsy, a piece of the mass or the entire mass is removed and tested for cancer.
It’s important to note that oftentimes a biopsy is not needed to rule in (or out) the diagnosis of liver cancer. This is because a CT scan and/or MRI can provide enough evidence that a mass is cancerous or not.
In this instance, avoiding a biopsy is ideal, as there is concern that removing cancerous cells from a mass may “seed” nearby areas with cancer. In that case, a spread of cancer may make a person ineligible for a liver transplant (a potential treatment option).
Regardless, sometimes a biopsy is necessary in order to make the diagnosis if imaging is not conclusive.
Differential Diagnosis
It's important to mention that a cancerous lesion in the liver may not be primary liver cancer but rather a metastatic lesion from another cancer. For example, colon cancer that spreads to the liver is called metastatic colon cancer or secondary liver cancer.6 In this case, your healthcare provider will need to investigate what the primary cancer is, if not known.
Furthermore, know that there are many potential diagnoses for a liver mass, meaning it's not necessarily cancer.
Two examples of benign (noncancerous) causes of liver masses include:7
Hepatic Hemangioma
Hepatic hemangioma is a mass of blood vessels that is the most common type of benign liver mass. It does not usually cause symptoms, but may cause abdominal discomfort, bloating, or early satiety if it becomes large enough. While a hepatic hemangioma does not usually require treatment, it may need to be removed by a surgeon if it breaks open and bleeds, although this is rare.
Hepatic Adenoma
A hepatic adenoma is a benign liver tumor that usually causes no symptoms unless it bleeds or grows large enough. In a small percentage of cases, a hepatic adenoma may turn into liver cancer, which is why it's generally removed.
Sources
Dimitroulis D, Damaskos C, Valsami S, et al. From diagnosis to treatment of hepatocellular carcinoma: An epidemic problem for both developed and developing world. World J Gastroenterol. 2017;23(29):5282-5294. doi:10.3748/wjg.v23.i29.5282
National Organization for Rare Disorders. Hepatocellular Carcinoma.
Bacon BR, Adams PC, Kowdley KV, Powell LW, Tavill AS; American Association for the Study of Liver Diseases. Diagnosis and management of hemochromatosis: 2011 practice guideline by the American Association for the Study of Liver Diseases. Hepatology. 2011;54(1):328-343. doi:10.1002/hep.24330
Hann HW, Wan S, Myers RE, et al. Comprehensive analysis of common serum liver enzymes as prospective predictors of hepatocellular carcinoma in HBV patients. PLoS One. 2012;7(10):e47687. doi:10.1371/journal.pone.0047687
Attwa MH, El-Etreby SA. Guide for diagnosis and treatment of hepatocellular carcinoma. World J Hepatol. 2015;7(12):1632-1651. doi:10.4254/wjh.v7.i12.1632
Valderrama-Treviño AI, Barrera-Mera B, Ceballos-Villalva JC, Montalvo-Javé EE. Hepatic Metastasis from Colorectal Cancer. Euroasian J Hepatogastroenterol. 2017;7(2):166-175. doi:10.5005/jp-journals-10018-1241
Heiken JP. Distinguishing benign from malignant liver tumours. Cancer Imaging. 2007;7 Spec No A(Special issue A):S1-S14. doi:10.1102/1470-7330.2007.9084
American Cancer Society. Liver cancer survival rates.
American Cancer Society. Signs and symptoms of liver cancer.
Additional Reading
American Cancer Society. Tests for Liver Cancer.
Bruix J, Sherman M, American Association for the Study of Liver Diseases. Hepatology. 2011 Mar;53(3):1020-2. dx.doi.org/10.1002/hep.24199
Schwartz JM, Carithers RL. (2017). Clinical features and diagnosis of primary hepatocellular carcinoma. Chopra S, ed. UpToDate. Waltham, MA: UpToDate Inc.
By Colleen Doherty, MD
Dr. Doherty is a board-certified internist and writer living with multiple sclerosis. She is based in Chicago.






Post comments